Photo from wikipedia
A 72-year-old woman presented to hospital with fever, lower abdominal pain, haematuria and hypotension. Her background was significant for deceased donor kidney transplantation over 20 years ago on the left… Click to show full abstract
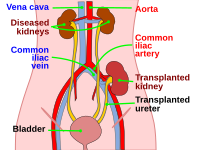
A 72-year-old woman presented to hospital with fever, lower abdominal pain, haematuria and hypotension. Her background was significant for deceased donor kidney transplantation over 20 years ago on the left side complicated by graft failure. Four years ago, she had repeat kidney transplantation on the right side. Her original transplant kidney was anastomosed to her native left external iliac artery (EIA). Urgent computed tomography (CT) scan revealed large-volume haemoperitoneum associated with a mycotic left EIA pseudoaneurysm communicating with her historic left transplant kidney (Fig. 1). The patient was resuscitated and emergently taken to the operating theatre where a 10 × 59 mm Viabahn VBX (balloonexpandable, Gore Medical, Flagstaff, Arizona, United States of America) stent was deployed percutaneously in the left EIA for haemorrhage control (Fig. 2). She was admitted to the intensive care unit for haemodynamic support. Intravenous (IV) ceftazidime was commenced for Pseudomonas aeruginosa bacteraemia. Her renal function (Cr 68 μmol/L) and haemoglobin (86 g/L) remained stable. Two days later, the patient underwent left transplant nephrectomy with ligation of the left common iliac artery (CIA) and a right to left femoral–femoral crossover bypass graft using cadaveric iliac artery for lower limb revascularization. The native left common iliac vein was ligated due to adherence to the transplant kidney capsule. Several small bowel enterotomies were made due to extensive adhesions requiring adhesiolysis, segmental small bowel resection and anastomosis. She spent 48 h in the intensive care unit for inotropic support and completed 5 days of oral metronidazole due to potential bowel contamination. The patient was anticoagulated with enoxaparin and then warfarin following common iliac vein ligation due to venous congestion and thrombus. Interval CT scan showed reduction in size of the pelvic haematoma and the patient was discharged 3 weeks post-operatively after completing 2 weeks of IV ceftazidime. Two weeks post discharge, the patient represented with abdominal pain and fever. CT scan showed a mycotic 41-mm pseudoaneurysm at the stump of the ligated left CIA (Fig. 3) from the presumed P. aeruginosa. A reversed aorto-uni right iliac stent graft (Gore Excluder, 16 × 23 × 120 mm) was deployed percutaneously in the distal aorta with distal seal in the right CIA (Fig. 3). The patient was discharged 11 days post admission on 6 weeks of IV meropenem followed by lifelong prophylactic ciprofloxacin following consultation with infectious disease and renal specialists. CT imaging 3 months post-operatively showed resolution of the right iliac stump collection and a patent aortic stent and femoral–femoral crossover graft. The patient remained clinically well and completed 12 months of warfarin once her left leg swelling had resolved. Mycotic arterial aneurysms have significant morbidity and mortality. Management consists of haemorrhage control, antibiotic therapy and surgical debridement with or without revascularization; therefore, the recommended management of mycotic renal transplant aneurysms is transplant nephrectomy with distal limb revascularization. Conduit choice for arterial bypass grafting is important in the setting of infection. If autologous vein is not available, then cadaveric vein may be preferable to a prosthetic conduit given its relative resistance to infection. Immunosuppression of patients receiving cadaveric allografts reduces aneurysmal breakdown by modifying host tolerance, thereby improving graft longevity. Immunosuppression also increases the risk of prosthetic graft infection. Using harvested autograft in our patient would increase operative time and morbidity, and given the patient was already immunosuppressed and had an infected field, the use of cadaveric graft was potentially the most appropriate option. Pseudomonas aeruginosa is a virulent organism, directly damaging arterial walls and has relative antibiotic resistance, so persistent vessel wall or graft infections and subsequent complications are more likely compared to more common pathogens such as viridans group Streptococcus. This necessitated the aggressive surgical explantation following endovascular treatment and initiation of lifelong antimicrobial therapy. The treatment of mycotic aneurysms has changed in the past decade with a shift to endovascular techniques as they are associated with lower morbidity compared to open surgery. They are a reasonable initial alternative in the haemodynamically unstable and often significantly co-morbid vascular patient where open surgery is highrisk. Some pathologies cannot be managed solely via an endovascular approach and so are managed in combination with open
Journal Title: ANZ Journal of Surgery
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!