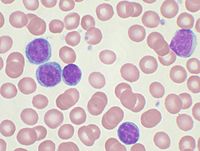
Photo from wikipedia
Identifying effective or synergistic combinations of targeted therapies and studying the tumour microenvironment (TME) are priority areas for lymphoma discovery and translation. This is particularly true for lymphoma patients who… Click to show full abstract
Identifying effective or synergistic combinations of targeted therapies and studying the tumour microenvironment (TME) are priority areas for lymphoma discovery and translation. This is particularly true for lymphoma patients who have more aggressive disease or harbour specific genetic markers [e.g. del(17p) or TP53 mutations in chronic lymphocytic leukaemia (CLL)]. CLL tumour cells depend on survival and proliferative signals that they receive through understudied interactions with surrounding stromal and immune cells within the TME (lymph node and bone marrow tissue). CLL cells are believed to proliferate within lymph node pseudofollicles or ‘proliferation centres’, where tumour B cells co-localise with CD4 helper T cells, macrophages, endothelial cells and mesenchymal-derived stromal cells (Kipps et al, 2017). B-cell receptor (BCR) engagement within the TME has emerged as a central oncogenic pathway essential for CLL survival and proliferation. The importance of this antigen interaction is underscored by the clinical success of kinase inhibitors that block BCR signalling (Burger & Wiestner, 2018). Within the TME or proliferation centres, CLL cells are exposed to antigens, extracellular matrix (ECM), integrins, chemokines, cytokines and growth survival factors that activate critical signalling pathways, including the BCR, Tolllike receptor signalling and canonical nuclear factor-ΚB pathways (Herishanu et al, 2011). Cellular interactions and exchange of soluble factors within the TME not only play a role during cancer progression but are also likely to profoundly affect therapeutic efficacy [‘TME-mediated resistance’ or, in other contexts, enhancement of therapeutic efficacy (Ramsay, 2013)]. The development and use of reliable models that mimic crosstalk between lymphoma cells and tissue-specific TME cellular and matrix components will be essential tools for interrogating disease biology as well as experimental therapeutics. Given that many of the pro-survival and proliferative pathways in CLL converge upon the mitogen-activated protein kinase or extracellular signal-regulated kinase (MAPK/ERK) signal transduction pathway (also known as the Ras-Raf-MEKERK pathway), this represents an attractive target within the CLL TME. Although inhibitors targeting Raf are efficacious for the treatment of melanoma (albeit linked to a high rate of secondary malignancy), the testing of Raf inhibitors in CLL has been challenging in the highly competitive clinical trial arena. However, a pre-clinical paper in this issue (Crassini et al, 2018) has investigated the inhibition of MEK1/2 using binimetinib as a novel therapeutic agent for CLL. The study demonstrates that binimetinib blocks microenvironment-induced activation of ERK signalling. Notably, in order to experimentally test TME crosstalk and the effect of therapy, the study utilised in vitro coculture models that exposed CLL tumour cells to recombinant SDF1-a (secreted or displayed by lymphoid stromal cells), antiIgM to ligate the BCR or conditioned media (secreted factors) from a bone marrow mesenchymal-derived stromal cell line. Interestingly, and in common with sorafenib (inhibitor of tyrosine kinases including Raf), TME-activated CLL cells were more sensitive to binimetinib than unstimulated CLL cells – highlighting the need to model TME signalling. Binimetinib also exhibited cytostatic activity against cycling primary CLL cells that had been stimulated with CpG-oilgonucletide in combination with interleukin (IL)-2 to activate Toll-like receptor and MAPK/ERK signalling and trigger cell-cycle progression. However, no cytotoxic effect towards tumour B cells was detected when CLL cells were co-cultured in direct contact with mesenchymal stromal cells, which was associated with increased levels of phosphorylated AKT in tumour cells. This finding is in keeping with previous studies demonstrating that CLL cells cocultured with bone marrow stromal cells are rescued from drug-induced apoptosis in a mechanism that is amplified following direct cell-cell contact (Kay et al, 2007). As the PI3kinase/AKT and MAPK/ERK pathways are known to regulate expression of the BCL-2 family proteins, the study hypothesised that combining binimetinib with BCL-2 inhibitors may overcome resistance. Venetoclax is a small molecule inhibitor that functions as a BH3 mimetic to inhibit BCL-2. This drug is highly potent in inducing apoptosis in CLL tumour cells including relapsed and del(17p) disease, (Roberts et al, 2016) but Correspondence: Dr Alan G. Ramsay, King’s College London, The Rayne Institute, 123 Coldharbour Lane, London SE5 9NU, UK. E-mail: [email protected] editorial comment
Journal Title: British Journal of Haematology
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!