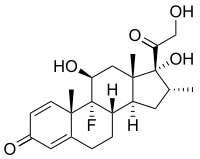
Photo from wikipedia
Corticosteroids are used in first‐line treatment in newly diagnosed immune thrombocytopenia. The goal of treatment is primarily to decrease autoantibody‐mediated platelet clearance. Ideally initial treatment would not just increase the… Click to show full abstract
Corticosteroids are used in first‐line treatment in newly diagnosed immune thrombocytopenia. The goal of treatment is primarily to decrease autoantibody‐mediated platelet clearance. Ideally initial treatment would not just increase the platelet count but also provide a long‐term sustained remission. While many clinicians use prednisone (PDN) as their first choice of corticosteroid, others prefer dexamethasone. The controversy is the subject of debates. Short courses of higher‐dose corticosteroids were first reported by the Andersen study in 1994. The study posited high‐dose dexamethasone as a ‘cure’ for all ITP patients. Later, studies addressed the number of dexamethasone cycles, indications to repeat cycles and timing between cycles, with varied long‐term results. The results with dexamethasone were compared to PDN in some studies: the four‐day cycles of dexamethasone work faster in increasing platelet counts and appear to reduce the occurrence of severe adverse events. Therefore, it is probably a better option for patients with low platelet counts and bleeding diathesis; however, curative superiority, the initial reason to administer it, compared to PDN is not well demonstrated. Across the studies, treatment with high‐dose dexamethasone seems to be safer, with lower incidence of all adverse events compared to PDN, which might be a reflection of shorter treatment duration and possibly also lower cumulative steroid dose. Dexamethasone in combination with rituximab in first‐line treatment produced higher response rates with better long‐term results compared to high‐dose dexamethasone alone and is a particularly good option in younger women.
Journal Title: British Journal of Haematology
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!