Photo from wikipedia
Galli–Galli disease (GGD) is a rare autosomal dominant genodermatosis, which is considered an acantholytic variant of Dowling–Degos disease (DDD). It is characterized by reticular, lentigo-like hyperpigmentation on the groins, axillae… Click to show full abstract
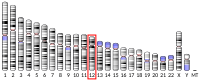
Galli–Galli disease (GGD) is a rare autosomal dominant genodermatosis, which is considered an acantholytic variant of Dowling–Degos disease (DDD). It is characterized by reticular, lentigo-like hyperpigmentation on the groins, axillae and large folds, occurring between puberty and early adulthood. Histology shows increased pigmentation of the basal layer, acanthosis with moderate to severe acantholysis, and finger-like rete ridges that result in antler-like patterns of epidermal downgrowths. Despite the presence of acantholysis, skin fragility has not been observed. There is no curative treatment for GGD, but symptoms may be managed by topical corticosteroids, topical and systemic retinoids, intense pulsed light or ablative laser therapy. The aforementioned clinical presentation corresponds to the DDD1 (OMIM 179850) variant caused by KRT5 mutations. Several mutations have been identified in the first exon of KRT5, all of which lead to premature termination codons (PTC), both in sporadic and familial cases. Most cases were reported from Germany, in which c.418dupA was described as the most common mutation in patients with acantholytic DDD. Further mutations were described in Spanish, Arabic, Asian-American, Chinese and Indian patients. In some cases, acantholysis was not observed, and it has also been reported that acantholysis may not necessarily be present at all times or at all anatomical sites. In many cases, both from Europe and Asia, an association between DDD/ GGD and a KRT5 mutation could not be detected. Recently, novel mutations in the POGLUT1 and POFUT1 genes of the Notch signalling pathway have also been identified as causative of DDD in German and Chinese familial and sporadic cases. A 74-year-old Hungarian man presented with a 30year history of a slowly progressing skin condition. Physical examination revealed poikiloderma and widespread pigmented lesions on the patient’s neck and trunk, and on the flexor surfaces of the extremities with small hypopigmented papules, and hyperpigmented macules, which occasionally became inflamed, forming psoriasiform papules over the reticular pattern (Fig. 1a). The patient’s father, grandfather and two brothers had the same ‘ocelot-like’ skin. Histopathology revealed increased pigmentation of the basal layer, finger-like rete ridges in the suprapapillary epidermis, and presence of acantholysis (Fig. 1c,d). A diagnosis of GGD was suggested. Both the inflamed skin condition and pigmentation improved significantly after the introduction of acitretin 25 mg daily (Fig. 1b), which was later reduced to 25 mg alternate daily. When the therapy was temporarily discontinued, the lesions suddenly worsened. Following ethics approval and informed consent, genetic analysis was performed. A heterozygous duplication of the base 418 of KRT5 was found, which causes a frameshift mutation resulting in a PTC in codon 179 (c.418dupA; p.Ile140AsnfsX39; Fig. 1e). This is the first Hungarian case of GGD with a clear genetic background. The KRT5 mutation c.418dupA (p.Ile140AsnfsX39) has been previously identified by Hanneken et al. as being the most common mutation Correspondence: Dr Norbert M. Wikonk al, Department of Dermatology, Venereology and Dermato-oncology, Semmelweis University, 41 M aria Street, 1085 Budapest, Hungary E-mail: [email protected]
Journal Title: Clinical and Experimental Dermatology
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!