Photo from wikipedia
A 71-year-old female patient presented in our Dermatology department with a 2-week history of pruritic lesions initially occurring on her upper trunk (Fig. 1a). Later, with the progression of the… Click to show full abstract
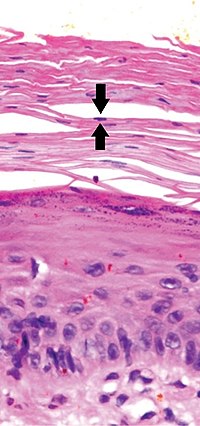
A 71-year-old female patient presented in our Dermatology department with a 2-week history of pruritic lesions initially occurring on her upper trunk (Fig. 1a). Later, with the progression of the disease, the patient noticed new lesions on the lower back and gluteal region, while the initial lesions remained unchanged. Lethargy and anorexia were associated symptoms. The patient had a medical history of autoimmune thyroiditis, chronic sinusitis, and chronic obstructive pulmonary disease. The clinical examination revealed large polycyclic edematous plaques with elevated erythematous-violaceous border and fading center (Fig. 1b). General physical examination did not show any other abnormalities. She denied a history of recent travel, infection, or initiation of a new drug or herbal preparation. We proceeded to skin biopsy of the border of one plaque, and the histologic examination showed perivascular and interstitial eosinophilic infiltrate with degenerative changes of connective tissue (Fig. 2). Neither granulomas nor “flame figures” were observed. Blood analysis revealed peripheral eosinophilia of 31% (absolute count 2604/ll), antimicrosomal antibodies 23.2 (1–16 UI/ml), but thyroid function showed normal values. The remainder of the immunology tests and the screening for infectious diseases were normal or negative. The patient was treated with oral prednisolone 0.5 mg/kg per day in a slow tapering schedule. Two weeks after initiation of corticosteroid therapy, we observed flattening of the lesions, leaving only residual hyperpigmentation. Due to excellent (a)
Journal Title: International Journal of Dermatology
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!