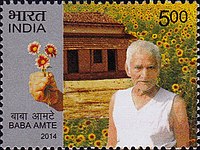
Photo from wikipedia
Pediatric leprosy: no child’s play Dear Editor, We read with interest the recent correspondence entitled “Childhood leprosy: a Pandora’s box.” The author reported a case of tuberculoid leprosy in a… Click to show full abstract
Pediatric leprosy: no child’s play Dear Editor, We read with interest the recent correspondence entitled “Childhood leprosy: a Pandora’s box.” The author reported a case of tuberculoid leprosy in a 5-year-old child. The diagnosis of childhood leprosy may be difficult due to both being uncommon and unusual presentations. Less than one-tenth of the total reported cases of leprosy are seen in children, and the proportion is even lower in children less than 5 years of age due to the long incubation period (3–5 years). Reactions are also rare in children, reported prevalence being 3.1–33.9%, compared with over 50% in adults. Uncommon occurrence of the disease and also lepra reactions in children should only make us more observant; these criteria, however, should not be used to label the case “unusual.” The significance of childhood leprosy cannot be understated. From an epidemiological point of view, it indicates continued transmission and a significant undiagnosed pool of disease in the community. Clinically, the disease may present a diagnostic and therapeutic challenge. From a psychosocial perspective, childhood leprosy may result in children being stigmatized and ostracized for life. We would, therefore, like to elaborate further upon certain aspects of this case, with emphasis on the holistic management of childhood leprosy. Certain clinical features like the proximal border of the lesion, in part, sloping and fading into the surrounding skin, a pseudopodium evident on the little finger, and the presence of type 1 (reversal) reaction suggestive of immunological instability pointed more toward the disease being in the borderline tuberculoid (BT) spectrum, which constitutes an overwhelming majority of childhood leprosy cases. Weight-based dosing of antileprosy treatment is recommended by the current guidelines in children younger than 10 years of age (rifampicin 10 mg/ kg/month, clofazimine 100 mg once a month and 50 mg twice weekly, and dapsone 2 mg/kg/day). Pediatric dosages are, however, not readily available through the national program, and providing the correct dosage is a challenge in most children, and this seems to hold true for the index case as well. Provision of pediatric drug preparations in the form of syrup or tablets is an aspect that deserves more attention in national programs. Prednisolone was started for type 1 reaction (T1R) but was stopped in 3 weeks. Current guidelines recommend the continuation of corticosteroids for 20 weeks in T1R due to the associated neural involvement. Adequate duration is especially important in children, as nerve function is difficult to evaluate, and the development of disability may vastly upsurge the disability-adjusted life years (DALYs). Another vital element omitted in this case is an examination of household and neighborhood contacts. Diagnosis of childhood leprosy provides a valuable opportunity for the detection of index cases in the family. In concordance with the World Health Organization guidelines, single-dose rifampicin (SDR) should be provided to all contacts (above 2 years of age, after excluding tuberculosis and leprosy) in the absence of contraindications. Bacillus Calmette–Guerin (BCG) vaccine is routinely administered in infancy in India. Cutaneous examination in a case of leprosy does include looking for BCG scar in the deltoid region. The protective efficacy of this vaccine is reported to be 26% in experimental studies and as high as 61% in observational studies. Failure to administer the BCG vaccine likely predisposed this child to develop leprosy. However, protection provided by BCG is not absolute, and it is more useful in preventing the occurrence of multibacillary rather than paucibacillary disease. To conclude, keeping with the paradigm “kids are not little people,” we highlight certain auxiliary attributes while managing a child with leprosy. A high index of suspicion and a careful examination are essential to reach the correct diagnosis. Weight-based dosing must be kept in mind while prescribing antileprosy treatment to avoid drug-related toxicities. Evaluation of contacts, chemoprophylaxis (SDR), and BCG vaccinations are of paramount significance in such cases. The absence of BCG vaccination brings in two more issues—the need for strengthening the vaccination program and also more stress on preventive health care—vaccinations being mostly free and are easily available in India.
Journal Title: International Journal of Dermatology
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!