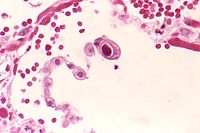
Photo from wikipedia
BACKGROUND AND OBJECTIVES Universal leucocyte depletion reduces the risk of transfusion transmitted Cytomegalovirus; however, many clinicians still prescribe Cytomegalovirus seronegative units. Our retrospective study aims to confirm the low risk… Click to show full abstract
BACKGROUND AND OBJECTIVES Universal leucocyte depletion reduces the risk of transfusion transmitted Cytomegalovirus; however, many clinicians still prescribe Cytomegalovirus seronegative units. Our retrospective study aims to confirm the low risk of transfusion transmitted Cytomegalovirus with leucocyte depletion alone and demonstrate the ongoing variability in Cytomegalovirus seronegative transfusion prescribing. MATERIALS AND METHODS Over a 9 year period (7/2009-7/2018), occurrences of transfusion transmitted Cytomegalovirus in Cytomegalovirus seronegative donor/recipient haemopoietic stem cell transplant pairs were compared at one allogeneic haemopoietic stem cell transplant centre providing Cytomegalovirus seronegative blood products and leucocyte depletion (double prevention) versus another providing leucocyte depletion only (single prevention). Retrospective chart audit identified patient demographics, blood product exposure and Cytomegalovirus infection by polymerase chain reaction. A separate audit examined Cytomegalovirus seronegative blood product ordering in a broader range of hospital types. RESULTS We identified 122 and 66 Cytomegalovirus negative donor/recipient haemopoietic stem cell transplant pairs using double and single transfusion prevention strategy respectively. Transfusion exposure to red cells and pooled platelets was similar, though more apheresis platelets were used in the double prevention group. Cytomegalovirus infection rate was 3 (2.4%) and zero in the double and single prevention groups respectively. Cytomegalovirus seronegative unit ordering was not limited to hospitals with obstetric or neonatal populations, suggesting ongoing reliance of Cytomegalovirus seronegative units outside this population. CONCLUSION The analysis suggests a double prevention strategy does not provide additional protection against transfusion transmitted Cytomegalovirus. There is ongoing variability in the acceptance of leucocyte depletion alone despite the low risk of Cytomegalovirus infection This article is protected by copyright. All rights reserved.
Journal Title: Internal medicine journal
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!