Photo from wikipedia
A recent study published in the Journal of the American Geriatrics Society reported that gabapentin and valproic acid are being increasingly prescribed to nursing home residents living with dementia, while… Click to show full abstract
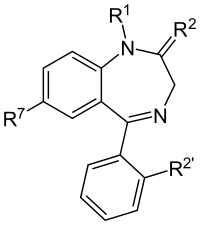
A recent study published in the Journal of the American Geriatrics Society reported that gabapentin and valproic acid are being increasingly prescribed to nursing home residents living with dementia, while at the same time, rates of antipsychotic prescribing are declining. This raises an important issue, one of a recurring pattern of off-label psychotropic substitutions to treat conditions such as behavioral and psychological symptoms of dementia (BPSD) and chronic pain in older adults. It also highlights how wellintentioned deprescribing efforts may result in the unintended consequence of increasing use of medications with similar harms and questionable benefits (Figure 1). A clear example of these unintended consequences can be found in the campaigns to reduce opioid use and the associated rise in gabapentinoid prescriptions. A recent study of US pharmacy claims showed that between 2006 and 2018, opioid prescribing episodes plateaued, while gabapentin prescribing episodes increased 5-fold from 1.5 to 8.1 million. Though gabapentin is often perceived as a safer alternative for pain management, the evidence for its efficacy is limited, especially in older adults. A 2020 systematic review and meta-analysis of randomized trials concluded there was low quality evidence for the effectiveness of gabapentinoids, and their analgesic and opioid-sparing effects may be clinically insignificant. These same clinical trials under-represented older adults, the patient population who are most vulnerable to the adverse effects of these drugs. This concern is reflected in the American Geriatrics Society's Beers Criteria, which lists gabapentin as a potentially inappropriate medication for older adults owing to its sedative properties and risk of respiratory depression. In 2022, a perioperative study demonstrated that gabapentin use by older adults within 2 days of surgery was associated with an increased risk of developing delirium and pneumonia. Considering of all this, we should be concerned that in our rush to address the opioid crisis, we have simply substituted other drugs that lack evidence and have known and increasingly documented risks of harm. Addressing antipsychotic use in nursing homes is another important medication stewardship effort that accelerated in 2005 when the Food and Drug Administration (FDA) issued a black box warning concerning increased risk of stroke and overall mortality for the use of antipsychotics in patients living with dementia. The American Geriatrics Society's Choosing Wisely Guidelines likewise recommends that antipsychotics should not be used as the first choice to treat BPSD. These warnings and guidelines accompanied increased public attention as See related article by Wastila et al. in this issue. Received: 15 February 2023 Revised: 14 March 2023 Accepted: 24 March 2023
Journal Title: Journal of the American Geriatrics Society
Year Published: 2023
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!