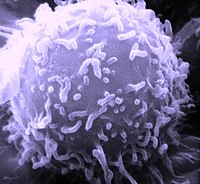
Photo from wikipedia
Characterization of the complex interplay between cytokines, chemokines and microorganisms has led to a better understanding of the pathogenesis of both psoriasis and AD and resulted in new therapeutics targeting… Click to show full abstract
Characterization of the complex interplay between cytokines, chemokines and microorganisms has led to a better understanding of the pathogenesis of both psoriasis and AD and resulted in new therapeutics targeting distinct immune responses. Psoriasis and AD share many characteristics: they are highly prevalent, chronic, cause primarily skin inflammation, but are associated with comorbidities, and come with a devastating quality of life due to itch and stigmatization. However, the pathogenesis of psoriasis and AD is opposing – psoriasis is dominated by a Th17 immune response that causes neutrophil migration, induction of innate immunity and exaggerated epithelial metabolism. Leading cytokines of this Th17 immune response are IL‐17A and F, IL‐22 and TNF‐a. AD is characterized by Th2 immunity characterized by the signature cytokines IL‐4 and IL‐13 leading to an impaired epidermal barrier, dampened innate immunity and eosinophil migration. This review compares genetics, microbiome and T‐cell infiltrate and resulting epithelial response in psoriasis and AD. Whilst the antagonistic course of psoriasis and AD is confirmed by response to specific biologics targeting the key cytokines of inflammation in psoriasis and AD, respectively, clinically overlapping phenotypes are challenging in our daily clinical practice. We conclude this review by summarizing what is known about these mixed phenotypes and how the identification of clinically relevant endotypes and molecular‐driven decision‐making is the next step in the field of dermato‐immunology.
Journal Title: Journal of Internal Medicine
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!