Photo from wikipedia
Antiphospholipid syndrome (APS) has been an enigma for many years. The diagnosis of a patient is based on rather generally occur‐ ring clinical symptoms in combination with specific laboratory tests.… Click to show full abstract
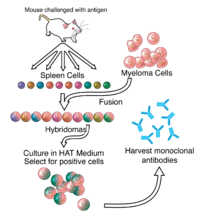
Antiphospholipid syndrome (APS) has been an enigma for many years. The diagnosis of a patient is based on rather generally occur‐ ring clinical symptoms in combination with specific laboratory tests. In more detail, as stated in its criteria, it is a syndrome in which pa‐ tients suffer from thrombosis and pregnancy morbidity.1 Diagnosis should be made on the basis of these clinical criteria in combination with laboratory criteria. Patients are tested positive for one or more of the following tests: anti‐beta2 glycoprotein‐1 (β2GP1) IgM/IgG antibodies, anti‐cardiolipin IgM/IgG antibodies, or prolongation of the phospholipid‐dependent coagulation time. Recently, the group of Devreese, together with our group, initiated a multicenter study in order to investigate whether we can improve the diagnosis of APS.2 Over the years, many groups have studied different popula‐ tions of antiphospholipid antibodies and their effect in initiating a prothrombotic phenotype. Many mechanisms have been proposed. Antibodies have been shown in vitro and in vivo to affect almost any protein or cell that is involved in the occurrence of thrombosis (Table 1).3 At present, the complement system is gaining attention as one of the major pathogenic mechanisms.4 As many mechanisms have been proposed to be involved in APS, it is quite difficult to choose a protein or cell to target for treatment. With this in mind, the idea of the group of Hisada et al is rather well thought out.4 Their main study objective was to identify the mech‐ anism of antiphospholipid antibody production. Study and identifi‐ cation of which cells are involved may make targeting of these for treatment an option. Interestingly, they found that the primary cells involved in antibody production were plasmablasts, which are the earliest plasma cells capable of producing antibodies. Characteristics of these cells are that they can divide rapidly, and that they are capable of internalizing antigens, presenting antigens to T cells, and producing antibodies. In fact, these cells are capable of producing high amounts of IgG antibodies. In addition, the authors show that the subpopulation of isolated peripheral blood mononuclear cells (PBMCs) that are CD20‐negative are more relevant regarding the production of antiphospholipid an‐ tibodies than PBMCs that are CD20‐positive. Rituximab, a chimeric mAb used to treat autoimmune diseases, has been used in patients with APS.5 Rituximab binds CD20 and thereby silences CD20‐pos‐ itive B cells, preventing the production of autoimmune antibodies. Interestingly, trials with rituximab in patients with APS have shown contrasting results. The failure of these trials might be partially re‐ lated to the findings discussed above. Attempting to stop antibody production instead of preventing symptoms is not a new idea, as, already in 1998, the group of Iverson et al studied treatment options in this respect.6 Antiphospholipid antibodies have been shown to predominantly react with β2GP1. The first domain of β2GP1 was shown to interact with autoantibod‐ ies that were highly associated with thrombosis. In the early years when anti‐domain 1 antibodies were gaining popularity, La Jolla Pharmaceutical Company developed a treatment strategy based on domain 1 reactivity. It produced a domain 1 tetramer in order to produce immune tolerance at the B‐cell level. Unfortunately, this treatment has not reached the clinic. This might be because the pop‐ ulation of antiphospholipid antibodies is heterogeneous. Although only antibodies that bind β2GP1 have been included in the official criteria used to diagnose APS, even within the subpopulation of anti‐β2GP1 antibodies there is heterogeneity, as several different non‐continuous epitopes have been shown to react with antiphos‐ pholipid antibodies.7 At present, different groups are working on different aspects of APS. More and more is being discovered about the mechanisms by
Journal Title: Journal of Thrombosis and Haemostasis
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!