Photo from wikipedia
Approximately 60 years ago in England, phototherapy for neonatal hyperbilirubinemia was used in clinical practice. It was introduced in Japan approximately 50 years ago. At that time, the mechanism underlying… Click to show full abstract
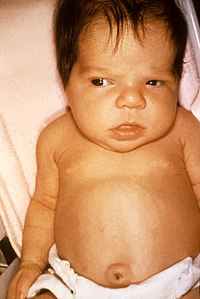
Approximately 60 years ago in England, phototherapy for neonatal hyperbilirubinemia was used in clinical practice. It was introduced in Japan approximately 50 years ago. At that time, the mechanism underlying the serum bilirubin concentration decrease by phototherapy was still unknown. The mechanism was identified by chemists, biochemists, and pediatricians. Clarification started with the report that unconjugated bilirubin was excreted into bile after photoirradiation in Gunn rats. After confirmation of the molecular structure of bilirubin on X‐ray analysis, the mechanism for bile excretion of unconjugated bilirubin was verified based on geometric configurational photoisomers in the Gunn rat. Finally, the reaction and excretion of structural bilirubin photoisomers was proved to be the main mechanism for the decrease in serum bilirubin during phototherapy for neonatal hyperbilirubinemia, which differs from the mechanism in the Gunn rat. The most effective and safest light source and the optimal method to evaluate phototherapy, however, remain unknown. Moreover, as for bronze baby syndrome, which is a well‐known adverse reaction to phototherapy, the etiology is unclear. Hence, we review phototherapy for hyperbilirubinemia including a fundamental understanding of the bilirubin photochemical reactions, and discuss the subclinical carcinogenic risk of phototherapy and the increased mortality rate of extremely low‐birthweight infants due to aggressive phototherapy, which is becoming an increasing problem.
Journal Title: Pediatrics International
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!