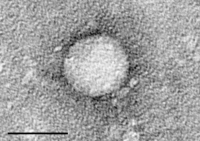
Photo from wikipedia
With new practice guidelines, it is important to understand how liver transplant (LT) centers have incorporated direct‐acting antivirals (DAAs) into the management of hepatitis C virus‐infected (HCV+) candidates and recipients.… Click to show full abstract
With new practice guidelines, it is important to understand how liver transplant (LT) centers have incorporated direct‐acting antivirals (DAAs) into the management of hepatitis C virus‐infected (HCV+) candidates and recipients. To explore how DAAs have affected LT centers’ willingness to treat HCV+ candidates and recipients and to use HCV+ donors, we surveyed high volume US LT centers (11/2014‐12/2015) regarding practices for HCV+ candidates, recipients, and donors, before vs after DAAs. We used the Scientific Registry of Transplant Recipients to compare centers’ number of LTs, HCV+ recipients, and HCV+ donors in the years before (1/1/2012‐12/31/2013) and after (1/1/2016‐12/31/2017) survey administration. Of 80 centers contacted, 57 (71.3%) responded, representing 69.0% of the total volume of LTs in 2013. After DAAs, most centers increased treating candidates with low (≤15) model for end‐stage liver disease (MELD) (85.2%), intermediate/high (>15) MELD (92.6%), and hepatocellular carcinoma (79.6%). There was consensus to treat low MELD candidates (90.8% “most of the time/always”), but less certainty for intermediate/high MELD candidates (48.2% “sometimes”). Universal post‐LT HCV treatment increased (7.4% vs 57.4%). After DAAs, 42.6% were more willing to use HCV+ donors for HCV+ candidates, and 38.9% were willing to consider using HCV+ donors for HCV− candidates. Overall, with DAAs, centers were more willing to treat HCV+ candidates and recipients and to use HCV+ donors; recent recommendations may help to guide treatment decisions for intermediate/high MELD candidates.
Journal Title: Transplant Infectious Disease
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!