Photo from wikipedia
Airborne volatile compounds produced by bacteria are often only considered attractive or repulsive scents, but they also directly contribute to bacterial physiology. Here, we showed that volatile hydrogen cyanide (HCN)… Click to show full abstract
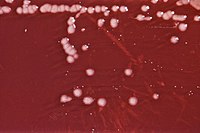
Airborne volatile compounds produced by bacteria are often only considered attractive or repulsive scents, but they also directly contribute to bacterial physiology. Here, we showed that volatile hydrogen cyanide (HCN) released by a wide range of Pseudomonas aeruginosa strains controls Staphylococcus aureus growth in low-oxygen in vitro biofilms or aggregates and in vivo lung environments. ABSTRACT Diverse bacterial volatile compounds alter bacterial stress responses and physiology, but their contribution to population dynamics in polymicrobial communities is not well known. In this study, we showed that airborne volatile hydrogen cyanide (HCN) produced by a wide range of Pseudomonas aeruginosa clinical strains leads to at-a-distance in vitro inhibition of the growth of a wide array of Staphylococcus aureus strains. We determined that low-oxygen environments not only enhance P. aeruginosa HCN production but also increase S. aureus sensitivity to HCN, which impacts P. aeruginosa-S. aureus competition in microaerobic in vitro mixed biofilms as well as in an in vitro cystic fibrosis lung sputum medium. Consistently, we demonstrated that production of HCN by P. aeruginosa controls S. aureus growth in a mouse model of airways coinfected by P. aeruginosa and S. aureus. Our study therefore demonstrates that P. aeruginosa HCN contributes to local and distant airborne competition against S. aureus and potentially other HCN-sensitive bacteria in contexts relevant to cystic fibrosis and other polymicrobial infectious diseases. IMPORTANCE Airborne volatile compounds produced by bacteria are often only considered attractive or repulsive scents, but they also directly contribute to bacterial physiology. Here, we showed that volatile hydrogen cyanide (HCN) released by a wide range of Pseudomonas aeruginosa strains controls Staphylococcus aureus growth in low-oxygen in vitro biofilms or aggregates and in vivo lung environments. These results are of pathophysiological relevance, since lungs of cystic fibrosis patients are known to present microaerobic areas and to be commonly associated with the presence of S. aureus and P. aeruginosa in polymicrobial communities. Our study therefore provides insights into how a bacterial volatile compound can contribute to the exclusion of S. aureus and other HCN-sensitive competitors from P. aeruginosa ecological niches. It opens new perspectives for the management or monitoring of P. aeruginosa infections in lower-lung airway infections and other polymicrobial disease contexts.
Journal Title: mBio
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!