Photo from wikipedia
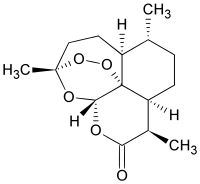
Malaria elimination is a Millennium Development Goal. Artemisinins, fast-acting antimalarial drugs, have played a key role in malaria elimination. ABSTRACT Emerging resistance to artemisinin drugs threatens the elimination of malaria.… Click to show full abstract
Malaria elimination is a Millennium Development Goal. Artemisinins, fast-acting antimalarial drugs, have played a key role in malaria elimination. ABSTRACT Emerging resistance to artemisinin drugs threatens the elimination of malaria. Resistance is widespread in South East Asia (SEA) and Myanmar. Neighboring Bangladesh, where 90% of infections occur in the Chittagong Hill Tracts (CHTs), lacks recent assessment. We undertook a prospective study in the sole district-level hospital in Bandarban, a CHT district with low population densities but 60% of reported malaria cases. Thirty patients presented with malaria in 2018. An increase to 68 patients in 2019 correlated with the district-level rise in malaria, rainfall, humidity, and temperature. Twenty-four patients (7 in 2018 and 17 in 2019) with uncomplicated Plasmodium falciparum monoinfection were assessed for clearing parasites after starting artemisinin combination therapy (ACT). The median (range) time to clear half of the initial parasites was 5.6 (1.5 to 9.6) h, with 20% of patients showing a median of 8 h. There was no correlation between parasite clearance and initial parasitemia, blood cell counts, or mutations of P. falciparum gene Pfkelch13 (the molecular marker of artemisinin resistance [AR]). The in vitro ring-stage survival assay (RSA) revealed one (of four) culture-adapted strains with a quantifiable resistance of 2.01% ± 0.1% (mean ± standard error of the mean [SEM]). Regression analyses of in vivo and in vitro measurements of the four CHT strains and WHO-validated K13 resistance mutations yielded good correlation (R2 = 0.7; ρ = 0.9, P < 0.005), strengthening evaluation of emerging AR with small sample sizes, a challenge in many low/moderate-prevalence sites. There is an urgent need to deploy multiple, complementary approaches to understand the evolutionary dynamics of the emergence of P. falciparum resistant to artemisinin derivatives in countries where malaria is endemic. IMPORTANCE Malaria elimination is a Millennium Development Goal. Artemisinins, fast-acting antimalarial drugs, have played a key role in malaria elimination. Emergence of artemisinin resistance threatens the global elimination of malaria. Over the last decade, advanced clinical and laboratory methods have documented its spread throughout South East Asia and Myanmar. Neighboring Bangladesh lies in the historical path of dissemination of antimalarial resistance to the rest of the world, yet it has not been evaluated by combinations of leading methods, particularly in the highland Chittagong Hill Tracts adjacent to Myanmar which contain >90% of malaria in Bangladesh. We show the first establishment of capacity to assess clinical artemisinin resistance directly in patients in the hilltops and laboratory adaptation of Bangladeshi parasite strains from a remote, sparsely populated malaria frontier that is responsive to climate. Our study also provides a generalized model for comprehensive monitoring of drug resistance for countries where malaria is endemic.
Journal Title: mBio
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!