Photo from wikipedia
Handling the infections by extensively drug-resistant Pseudomonas aeruginosa (XDRPA) strains is challenging due to their complicated antibiotic resistance mechanisms in immunosuppressed patients with pulmonary diseases (e.g., cystic fibrosis, chronic obstructive… Click to show full abstract
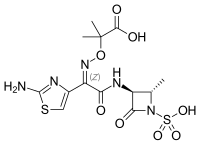
Handling the infections by extensively drug-resistant Pseudomonas aeruginosa (XDRPA) strains is challenging due to their complicated antibiotic resistance mechanisms in immunosuppressed patients with pulmonary diseases (e.g., cystic fibrosis, chronic obstructive pulmonary disease, and lung transplant), ventilator-associated pneumonia, and bloodstream infections. The current study suggested the potentiality of the ceftazidime-avibactam-imipenem combination against XDRPA with blaAmpC overexpression or mutation, decreased OprD porin, and/or upregulated efflux pumps. ABSTRACT Extensively drug-resistant Pseudomonas aeruginosa (XDRPA) infection is a significant public health threat due to a lack of effective therapeutic options. New β-lactam-β-lactamase inhibitor combinations, including ceftazidime-avibactam (CZA), have shown a high resistance rate to XDRPA. This study was therefore conducted to describe the underlying genomic mechanism of resistance for CZA nonsusceptible XDRPA strains that are non-metallo-β-lactamase (MBL) producers as well as to examine synergism of CZA and other antipseudomonal agents. Furthermore, the synergistic antibacterial activity of the most effective antimicrobial combination against non-MBL-producing XDRPA was evaluated through in vitro experiments. The resistance profiles of 15 CZA-resistant XDRPA strains isolated from clinical specimens in China-Japan Friendship Hospital between January 2017 to December 2020 were obtained by whole-genome sequencing (WGS) analysis. MBL genes blaIMP-1 and blaIMP-45 were found in 2 isolates (2/15, 13.3%); the other underlying CZA-resistance mechanisms involved the decreased OprD porin (13/13), blaAmpC overexpression (8/13) or mutation (13/13), and upregulated efflux pumps (13/13). CZA-imipenem (CZA-IPM) combination was identified to be the most effective against non-MBL-producing XDRPA according to the results of WGS analysis and combined antimicrobial susceptibility tests, with an approximately 16.62-fold reduction in MICs compared to CZA alone. Furthermore, the results of checkerboard analysis and growth curve displayed the synergistic antimicrobial activity of CZA and IPM against non-MBL-producing XDRPA. Electron microscopy also revealed that CZA-IPM combination might lead to more cellular structural alterations than CZA or IPM alone. This study suggested that the CZA-IPM combination has potential for non-MBL-producing XDRPA with blaAmpC overexpression or mutation, decreased OprD porin, and upregulated efflux pumps. IMPORTANCE Handling the infections by extensively drug-resistant Pseudomonas aeruginosa (XDRPA) strains is challenging due to their complicated antibiotic resistance mechanisms in immunosuppressed patients with pulmonary diseases (e.g., cystic fibrosis, chronic obstructive pulmonary disease, and lung transplant), ventilator-associated pneumonia, and bloodstream infections. The current study suggested the potentiality of the ceftazidime-avibactam-imipenem combination against XDRPA with blaAmpC overexpression or mutation, decreased OprD porin, and/or upregulated efflux pumps. Our findings indicate the necessity of combined drug sensitivity tests against XDRPA and also lay a foundation for the development of prevention, control, and treatment strategies in XDRPA infections.
Journal Title: Microbiology Spectrum
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!