Photo from wikipedia
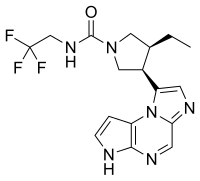
Background Upadacitinib (UPA), an oral JAK inhibitor, showed efficacy in rheumatoid arthritis (RA) patients (pts) with an inadequate response to csDMARDs or bDMARDs on continuing stable csDMARD(s).1 2 Objectives Safety… Click to show full abstract
Background Upadacitinib (UPA), an oral JAK inhibitor, showed efficacy in rheumatoid arthritis (RA) patients (pts) with an inadequate response to csDMARDs or bDMARDs on continuing stable csDMARD(s).1 2 Objectives Safety and efficacy of switching to UPA 15 mg or 30 mg monotherapy vs continuing methotrexate (MTX) as a blinded study drug was evaluated in pts with inadequate response to MTX (MTX-IR). Methods Pts with active RA (TJC ≥6, SJC≥6, hsCRP ≥3 mg/L) on stable MTX were enrolled and randomised 1:1:1 in a double-blind manner to once-daily (QD) UPA 15 mg or 30 mg monotherapy or to continue MTX (cMTX) at their prior stable dose. At BL, all pts discontinued prior MTX without washout and received PBO (for pts on UPA) or MTX at prior dose (cMTX) as blinded study drug. The primary endpoints at Week (Wk) 14 were the proportion of pts achieving ACR20, and the proportion achieving DAS28-CRP≤3.2 (NRI). Results 648 pts were randomised, all received study drug; 598 (92.3%) completed 14 wks. BL demographics and disease characteristics were generally similar across arms. Both primary endpoints were met (p<0.001); at Wk 14, a significantly greater proportion of pts receiving UPA monotherapy (15 mg and 30 mg) vs cMTX achieved ACR20 (67.7% and 71.2% vs 41.2%), and DAS28-CRP≤3.2 (44.7% and 53.0% vs 19.4%) (table 1). All key secondary endpoints also showed UPA 15 and UPA 30 monotherapy to be superior to cMTX, including ACR50 (41.9% and 52.1% vs 15.3%), ACR70 (22.6% and 33.0% vs 2.8%), DAS28-CRP<2.6 (28.1% and 40.5% vs 8.3%), ΔHAQ-DI (−0.65 and −0.73 vs −0.32). ΔSF-36 PCS and ΔMorning Stiffness data are also shown (table 1). The proportion of pts achieving CDAI≤10 was significantly greater with UPA 15 and 30 vs cMTX (34.6% and 46.5% vs 24.5%). Adverse events (AEs) were reported at similar frequencies across arms; serious AEs were numerically higher in UPA 15 but similar between cMTX and UPA 30 (table 1). Numerically more infections were reported in cMTX and UPA 30 vs UPA 15. One serious infection each was reported in UPA 15 and cMTX, and none in UPA 30. Herpes zoster was more frequent in UPA 30 vs UPA 15 or cMTX. 3 malignancies (1 in cMTX and 2 in UPA 15) and 3 adjudicated MACE (1 in UPA 15 and 2 in UPA 30) were reported. One adjudicated pulmonary embolism was reported (UPA 15) in a pt with known risk factors (BMI 36; on oestrogen therapy). One death (haemorrhagic stroke due to ruptured aneurysm) was reported in UPA 15. No TB, renal dysfunction or GI perforation was reported. Rates and types of laboratory abnormalities were consistent with prior UPA RA studies to date.Abstract OP0035 – Table 1 Conclusions In this MTX-IR study population, switching to UPA as monotherapy at 15 mg and 30 mg QD showed significant improvements in RA signs and symptoms vs continuing MTX. Numerically higher responses were observed for UPA 30 mg vs 15 mg, particularly for more stringent efficacy criteria. Safety observations were similar to those in prior UPA studies. References [1] Burmester, et al. Arth Rheum2017;69:S10. [2] Genovese, et al. Arth Rheum2017;69:S10. Acknowledgements AbbVie: Study sponsor, study design, data collection, analysis and interpretation, writing, review, approval of final. Medical writing:Naina Barretto of AbbVie Disclosure of Interest J. Smolen Grant/research support from: AbbVie, Consultant for: AbbVie, S. Cohen Grant/research support from: Abbvie, Gilead, Eli Lilly,Pfizer, Consultant for: Abbvie, Gilead, Eli Lilly,Pfizer, P. Emery Grant/research support from: Pfizer, MSD, AbbVie, Bristol-Myers Squibb, UCB, Roche, Novartis, Samsung, Sandoz and Lilly., Consultant for: Pfizer, MSD, AbbVie, Bristol-Myers Squibb, UCB, Roche, Novartis, Samsung, Sandoz and Lilly., W. Rigby: None declared, Y. Tanaka Grant/research support from: Mitsubishi-Tanabe, Takeda Ltd, BMS, Chugai Ltd, Astellas Inc, AbbVie GK, MSD K.K., Daiichi Sankyo Ltd, Pfizer Japan Inc., Kyowa Hakko Kirin, Ltd, Eisai., Ltd, Ono, Ltd, Speakers bureau: Daiichi Sankyo Ltd, Astellas Pharma Inc, Pfizer Japan Inc., Mitsubishi-Tanabe, BMS, Chugai Ltd, YL Biologics, Eli Lilly Japan KK, Sanofi KK, Janssen KK, UCB Japan, Ltd, Y. Zhang Shareholder of: AbbVie, Employee of: AbbVie, A. Friedman Shareholder of: AbbVie, Employee of: AbbVie, A. Othman Shareholder of: AbbVie, Employee of: AbbVie, H. Camp Shareholder of: AbbVie, Employee of: AbbVie, A. Pangan Shareholder of: AbbVie, Employee of: AbbVie
Journal Title: Annals of the Rheumatic Diseases
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!