Photo from wikipedia
© Author(s) (or their employer(s)) 2022. No commercial reuse. See rights and permissions. Published by BMJ. A previously healthy 22yearold man presented with bone and joint pain progressively increasing over… Click to show full abstract
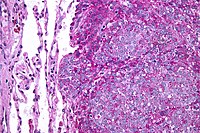
© Author(s) (or their employer(s)) 2022. No commercial reuse. See rights and permissions. Published by BMJ. A previously healthy 22yearold man presented with bone and joint pain progressively increasing over 12 months, localised on forearms and legs. One year before, he had suffered from desquamating skin lesions on both hands, which had spontaneously regressed. He had lost 10 kg since his first skeletal symptoms with no other general signs such as fever. There was no heel pain, dactylitis, psoriasis, transit disorder or genital infection preceding the symptoms. Clinical palpation reproduced bone and joint pain. No signs of systemic disease were found. Standard laboratory examinations showed an inflammatory syndrome with C reactive protein of 29 mg/L, erythrocyte sedimentation rate of 54 mm. Xrays of the long bones showed several focal cortical and medullary bone lytic lesions with periosteal reaction visible in middle parts of radius, ulna and tibias. There was a significant uptake in both tibias, parietal and occipital bones and mandible that matched with osteolytic lesions on bone scintigraphy. Positron emission tomography/CT scanner revealed areas of uptake in all tibias, radius and ulna (figure 1). Given this medical history and the radiological presentation, some hypotheses were discussed: SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome, Langerhans cell histiocytosis, tumorous diseases. Another hypothesis was syphilitic infection, based on the following features: the previous history of skin lesions, the fluctuating nature of symptoms and finally the topography of bone lesions in ulnas and tibias, strongly suggestive of syphilis. Diagnosis of syphilitic infection was, therefore, suspected, and laboratory tests revealed positive Treponema pallidum haemagglutination assay with levels of 24.62 (positive if ≥1) and veneral disease research laboratory (VDRL) test with ratio of 1/512, confirming the diagnosis of late syphilis with osteitis. The patient received three doses of longacting benzathin penicillin G intramuscularly (2.4 million units per injection) administrated at weekly intervals. Clinical response was quickly achieved after the first intramuscular injection and VDRL test rapidly decreased and was of 1/16 at 8 months. This clinical case highlights the importance of the new classification that distinguishes early syphilis from late syphilis arising after 1 year of evolution. Although syphilitic osteitis is rare, this diagnosis must be considered, even in young adults, especially as the incidence of syphilis is currently raising.
Journal Title: Annals of the Rheumatic Diseases
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!