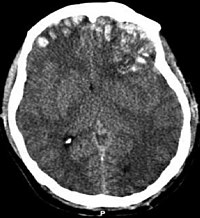
Photo from wikipedia
Background Several paediatric physiologically-based pharmacokinetic (PBPK) models have been developed that incorporate developmental changes affecting plasma drug concentrations. Disposition into cerebrospinal fluid (CSF) is also age-related and influenced by physiological… Click to show full abstract
Background Several paediatric physiologically-based pharmacokinetic (PBPK) models have been developed that incorporate developmental changes affecting plasma drug concentrations. Disposition into cerebrospinal fluid (CSF) is also age-related and influenced by physiological factors, including CSF production rate, but also by brain diseases, such as meningitis, which are associated with impaired blood-brain barrier integrity. Our aim was to develop a paediatric brain PBPK model to predict CSF drug concentrations in children with and without meningitis. Methods A paediatric PBPK model was developed incorporating age-appropriate parameters and associated inter-individual variability. The model was validated for paracetamol, ibuprofen, flurbiprofen and naproxen, and for a paediatric meningitis population by estimating meropenem blood-brain barrier penetration using sensitivity analysis. Plasma and CSF drug concentrations derived from literature were used to perform visual predictive checks and to calculate ratios between simulated and observed AUCs in order to evaluate model performance. Results Simulated data were comparable to observed over a broad age range (1 day - 15 y postnatal age), for all drugs investigated. The ratios between observed and simulated AUCs were within 2-fold difference both in plasma and in CSF, indicating acceptable model performance. Disposition of meropenem into the brain was slow and CSF concentrations were lower compared to plasma concentrations. In addition, several days were needed to achieve CSF steady-state concentration. Conclusions Our paediatric brain PBPK model provides a new tool to predict CSF concentrations in children with and without meningitis and can be used as a template model for other drugs acting in the CNS. Disclosure(s) Nothing to disclose
Journal Title: Archives of Disease in Childhood
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!