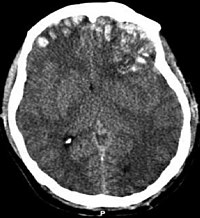
Photo from wikipedia
In 2014 the Royal College of Radiology published the ‘Paediatric Trauma Protocols’ emphasising ‘clinical evaluation…knowledge of injury patterns in children… judicious use of plain radiographs and targeted use of CT… Click to show full abstract
In 2014 the Royal College of Radiology published the ‘Paediatric Trauma Protocols’ emphasising ‘clinical evaluation…knowledge of injury patterns in children… judicious use of plain radiographs and targeted use of CT (Computed Tomography).’ There is ‘increasingly clear (evidence) that the cancer risk of CT in childhood is real.’ In 2016 our paediatric trauma imaging guidelines were updated. This study aims to identify if: The guidelines identify those sustaining pathology from trauma Following the guidelines with correct method of imaging identifies pathology. We can establish which methods of imaging best identify pathology caused by major trauma. Methods All trauma patients aged 0–16 at the major trauma centre over a 6 month period were identified. Retrospectively reviewing clinical records identified whether patients followed Head, C-Spine, Chest and Abdominal/Pelvic imaging guidelines; whether imaging identified pathology; and whether subsequent imaging beyond the ED identified missed injuries. Results 114 patients were identified. Head: PPV (Positive Predictive Value)=0.5 (95% CI 0.41–0.59), NPV (Negative Predictive Value)=1. 22 of 40 patients meeting criteria to be scanned had pathology. Correct guideline use identified 95% of pathology. One case was missed in the ED despite meeting criteria C–Spine: PPV=0.039 (0.032–0.048). NPV=1. 2 of 51 patients meeting criteria had pathology. It accurately identified 100% of pathology. No C–spine injuries were missed. Chest: PPV=0.24 (0.17–0.33), NPV=0.99 (0.93–1). 9 of 33 patients meting criteria had pathology. Accurate use identified 6 cases in ED. 2 cases were identified later (1 not meeting criteria to image; 1 normal imaging in ED). 1 child had CT instead of Chest X–Ray. Abdomen/Pelvis: PPV=0.33 (0.23–0.45), NPV=0.99 (0.93–1). 9 of 24 patients meeting criteria had pathology. Pelvic X–ray (PXR) is not recommended. 28 had PXR. One pelvic fracture was identified only on CT. One patient had pathology on CT despite not meeting guidelines for scan – an isolated L1/L2 fracture. Conclusions When assessing the need for imaging, all guidelines had high NPV’s. Low PPV’s (particularly C-spine) suggest we could consider tightening imaging criteria. No major injury requiring intervention was missed. Low rates of pathology and follow up imaging make it difficult to accurately assess the sensitivity and specificity of specific imaging techniques.
Journal Title: Archives of Disease in Childhood
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!