Photo from wikipedia
A 54yearold man presented with a 5day history of progressive leftsided neck pain, stiffness and odynophagia. There was no associated fever, history of trauma or airway compromise. The patient was… Click to show full abstract
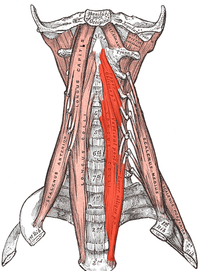
A 54yearold man presented with a 5day history of progressive leftsided neck pain, stiffness and odynophagia. There was no associated fever, history of trauma or airway compromise. The patient was fit and well with no medical history. Physical examination of the neck revealed severely reduced range of movement in all cervical planes. Oral cavity and neurological examinations were normal, and generalised pharyngeal oedema was seen on flexible nasendoscopy. The patient was apyrexial throughout with other physiological observations within normal limits. Only a mildly raised C reactive protein was noted on blood work. The patient was taken for urgent contrast CT neck, revealing a prevertebral fluid collection of unclear aetiology extending from the clivus to the inferior border of C5 (figure 1). An area of calcification was noted below the anterior arch of C1, in keeping with calcification at the superior insertion of the longissimus coli tendon(figure 2). To further evaluate these findings, MRI neck with contrast was performed 3 days later. This demonstrated a prevertebral fluid collection with enhancement extending down to level of the upper border of T2 and again revealing calcification in the left longus colli muscle. Along with the differential diagnosis of calcific tendonitis of longus colli (CTLC), the fluid collecting inferior to C1 could have represented a retropharyngeal abscess—a potentially lifethreatening infection. The imaging was reviewed with multiple specialities including radiology, otolaryngology, infectious diseases, neurosurgical and rheumatology teams; concluding that the most likely diagnosis was CTLC with associated oedema creating a fluid collection—supported by the clinical condition of the patient who remained well. Treatment was with regular nonsteroidal antiinflammatory medication with proton pump cover and physiotherapy. Other published cases have described the use of steroids, H2 antagonists, surgical intervention and cervical collars; however, there is little evidence to support their use. Current literature describes most CTLC cases to be selflimiting and resolve spontaneously in 1–2 weeks, as was the case here. Exact aetiology is unknown, however calcification may occur following injury or repetitive trauma, similar to that of calcific tendinitis in other locations. It later came to light that the patient had been performing extensive pruning of trees prior to presentation requiring prolonged periods of neck extension, while carrying heavy machinery, and episodes of sharp flexion to avoid falling branches. Although CTLC represents a benign and perhaps underrecognised condition, this case highlights the importance of considering other differential diagnoses in a patient presenting with limited neck movements. This patient was systemically well making a retropharyngeal abscess unlikely, however dismissing this could have had catastrophic consequences for the patient as an abscess would have required prompt airway management and surgical drainage. Literature has demonstrated the pathognomonic finding of prevertebral oedema associated with CTLC; however, the fluid collection seen here was not immediately characteristic and mimicked a more clinically concerning diagnosis of an abscess. Luckily for this patient, prompt recognition of Figure 1 Sagittal CT image showing superior and inferior extent of fluid collection in retropharyngeal space (yellow arrows) and calcification at insertion of longissimus coli (orange arrow).
Journal Title: BMJ Case Reports
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!