Photo from wikipedia
© BMJ Publishing Group Limited 2022. No commercial reuse. See rights and permissions. Published by BMJ. DESCRIPTION A man in his 30s with active consumption of cocaine, heroin and alcohol… Click to show full abstract
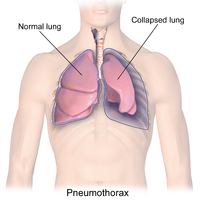
© BMJ Publishing Group Limited 2022. No commercial reuse. See rights and permissions. Published by BMJ. DESCRIPTION A man in his 30s with active consumption of cocaine, heroin and alcohol presented with progressive halfyear evolution of hoarseness, dysphonia, dysphagia (initially for solids, later for liquids), dyspnoea and cough, associated with fever, night sweats and significant weight loss (30–40 kg); he was in poor general condition, very thin and dehydrated. Laboratory tests revealed a lymphocytic leucocytosis with a marked increase in C reactive protein; arterial blood gas analysis showed type I respiratory failure; HIV test was negative. Nasopharyngolaryngoscopy revealed hypertrophy/hyperaemia of the pharyngolaryngeal mucosa from the epiglottis to the ventricular bands, making it impossible to assess the vocal cords. Chest CT demonstrated multiple cavitated lesions on the pulmonary parenchymal, the main lesion located in the right lung apex; it also revealed countless small, welldefined, centrilobular nodules connected to linear branching opacities, the socalled treeinbud appearance: typical findings of postprimary tuberculosis (TB) (figure 1). CT scan of the neck also showed a diffuse thickening and enhancement from the epiglottis to the hypopharynx and vocal cords, symmetrically, with no exophytic lesions (figure 2). Sputum smear microscopy–ZiehlNeelsen and auramine stains–revealed acidfast bacilli. Nucleic acid amplification tests were positive for Mycobacterium tuberculosis. Standard induction treatment was initiated with isoniazid (INH), rifampicin (RIF), pyrazinamide (PAZ) and ethambutol (EMB) and maintained for 2 months with favourable clinical response. Drug susceptibility was later confirmed, and subsequently there was a transition to the maintenance regimen with INH and RIF, continued for another 7 months. Once the therapeutic regimen was completed, there was an overall clinical improvement with minor residual hoarseness. Posttreatment nasopharyngolaryngoscopy showed no residual pathological changes. Radiological resolution was documented in crosssectional imaging, with few and small persistent lung cavities and very discreet right vocal cord thickening (figures 1 and 2). Pharyngolaryngeal tuberculosis (PLTB) was one of the most common extrapulmonary forms of the disease before the era of antibiotics. 2 Although the literature reports an annual incidence of 1%, its prevalence is increasing in some countries, mainly fuelled by HIV epidemics and immunosuppressive therapeutics. PLTB generally accompanies a pulmonary involvement, mostly from pooling of highly infectious sputum or even by haematogenous spread. 2 It affects men more commonly and it is often associated with heavy smoking and alcohol consumption. Figure 1 Chest CT, lung window: axial (A,B,D,E) and sagittal (C,F) sections before and after treatment (top and bottom rows, respectively). Presence of multiple cavitated lesions disperse on the pulmonary parenchymal, with the main lesion located in the right lung apex (A,D), and countless small, centrilobular nodules connected to linear branching opacities: treeinbud appearance (main imaging finding in B). After treatment, there is marked regression of the size of the cavitated lesions and disappearance of the treeinbud sign.
Journal Title: BMJ Case Reports
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!