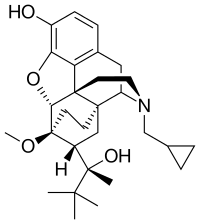
Photo from wikipedia
Objectives This study describes the 2016 expansion of the British Columbia Take Home Naloxone (BCTHN) programme quantitatively and explores the challenges, facilitators and successes during the ramp up from the… Click to show full abstract
Objectives This study describes the 2016 expansion of the British Columbia Take Home Naloxone (BCTHN) programme quantitatively and explores the challenges, facilitators and successes during the ramp up from the perspectives of programme stakeholders. Design Mixed-methods study. Setting The BCTHN programme was implemented in 2012 to reduce opioid overdose deaths by providing naloxone kits and overdose recognition and response training in BC, Canada. An increase in the number of overdose deaths in 2016 in BC led to the declaration of a public health emergency and a rapid ramp up of naloxone kit production and distribution. BCTHN distributes naloxone to the five regional health authorities of BC. Participants Focus groups and key informant interviews were conducted with 18 stakeholders, including BC Centre for Disease Control staff, urban and rural site coordinators, and harm reduction coordinators from the five regional health authorities across BC. Primary and secondary outcome measures Take Home Naloxone (THN) programme activity, qualitative themes and lessons learnt were identified. Results In 2016, BCTHN responded to a 20-fold increase in demand of naloxone kits and added over 300 distribution sites. Weekly numbers of overdose events and overdose deaths were correlated with increases in THN kits ordered the following week, during 2013–2017. Challenges elicited include forecasting demand, operational logistics, financial, manpower and policy constraints. Facilitators included outsourcing kit production, implementing standing orders and policy changes in naloxone scheduling, which allowed for easier hiring of staff, reduced paperwork and expanded client access. Conclusion For THN programmes preparing for potential increases in naloxone demand, we recommend creating an online database, implementing standing orders and developing online training resources for standardised knowledge translation to site staff and clients.
Journal Title: BMJ Open
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!