Photo from wikipedia
We read with interest the work by Jachs et al, reporting the benefits of nonselective beta blockers (NSBBs) in reducing systemic inflammation in individuals with cirrhosis, with an associated reduced… Click to show full abstract
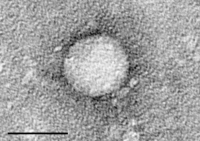
We read with interest the work by Jachs et al, reporting the benefits of nonselective beta blockers (NSBBs) in reducing systemic inflammation in individuals with cirrhosis, with an associated reduced rate of acute decompensation and mortality. Systemic inflammation is a hallmark of cirrhosisassociated immune dysfunction, representing pathological translocation of bacteria and/or bacterial products from the gut. Cirrhotics have an increased risk of developing infection, with substantially increased mortality when such infections occur. 5 Secondary infections significantly contribute to this, and predict 30day mortality independently of disease severity. 7 Extending on the work of Jachs et al, we here report a beneficial impact of NSBB on clinical and microbiological outcomes of decompensated cirrhotics in both a specialist outpatient setting and inpatients. We also report the novel finding of a reduction in circulating bacterial DNA (bDNA) levels in a subset of cirrhotics with primary infections on NSBB. We retrospectively analysed 138 patients with ChildPugh grade B/C cirrhosis attending a specialist cirrhosis outpatient clinic at St Mary’s Hospital, London, over a 2year period. Patients were included at the point of clinic attendance, with records of adverse events (including hospitalisation) and mortality collected from electronic notes. Baseline characteristics of this cohort are shown in table 1. The indication for NSBB for all patients in this cohort was for either primary or secondary prophylaxis of varices. NSBB use (89/138) was associated with improved survival (p=0.01), lower 1year incidence of infection requiring hospitalisation (p=0.03), and reduced need for allcause admission (p=0.02). On binary logistic regression; factors independently associated with 1year survival were NSBB use (OR 5.18, 95% CI 1.67 to 16.01, p=0.004), lower baseline Model For EndStage Liver Disease score (OR 1.25, 95% CI 1.11 to 1.41, p=0.0001) and lower infection rates (OR 1.72, 95% CI 1.17 to 2.58, p=0.007). Subsequently, we prospectively investigated the impact of NSBB use on bDNA levels and the 28day incidence of secondary infection. We assessed bDNA levels in 22 consecutive cirrhotics admitted with primary infection with followup at day 28. At this point, they were assessed for secondary infection development, defined as per the North American Consortium for the Study of EndStage Liver Disease criteria, with blood sampling for 16S rRNA gene count (bacterial DNA load) analysis using PCR. Further details are included in the online supplemental material. Of the 22 patients, 50% Letter
Journal Title: Frontline Gastroenterology
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!