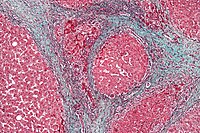
Photo from wikipedia
Introduction Splanchnic venous thromboses are recognised complication of acute and chronic pancreatitis. Splenic vein thrombosis (SVT), in isolation or in association with portal vein thrombosis (PVT) or superior mesenteric vein… Click to show full abstract
Introduction Splanchnic venous thromboses are recognised complication of acute and chronic pancreatitis. Splenic vein thrombosis (SVT), in isolation or in association with portal vein thrombosis (PVT) or superior mesenteric vein thrombosis (SMVT) can lead to collateral circulation and varices formation. Splanchnic varices are believed to be more problematic for patients with pancreatic pseudocysts (PP), although their true impact on this condition is not well described. The presence of varices within the peri-gastric operational field is potentially hazardous in patients undergoing endoscopic drainage. The aim of this study was to investigate the incidence of splanchnic varices, and evaluate their impact on clinical outcome of patients undergoing endoscopic ultrasound guided transmural drainage (EUD) of PP. Method A retrospective analysis of consecutive patients with symptomatic PP who underwent EUD between 2011 and 2016 was performed. Patients were identified from a prospectively collated database, with clinical data retrieved from patient records. Axial CT and MRI imaging performed in the four weeks prior to EUD was reviewed blindly by a specialist HPB radiologist. The primary outcome was to characterise the incidence of varices in patients with symptomatic PP. Secondary outcomes were to evaluate the technical success (ability to place the transmural stent), early and late adverse events (AE), and long term success (complete resolution of the cyst at 3 months) in patients with and without splanchnic varices. Results 117 patients (35% female; mean age 51 years) underwent EUD. Mean cyst size was 110 mm (30–220 mm). Venous thromboses were identified in 22 (18.8%) patients (isolated SVT=12, SVT+PVT=6, SVT+SMVT+PVT=3, isolated PVT=1). Splanchnic varices were present on radiological imaging in 69 (59%) patients. Anatomical distribution of varices was: gastro-splenic (72.5%), splenic (13%), gastric (1.5%), gastro-duodenal (1.5%), gastro-oesophageal (1.5%). Overall technical success rate of EUD was 76.1%. Intra-procedural complications were significantly higher in patients with varices (19% Vs 4%), p=0.02. Successful stent placement was higher in non-varices group (79% Vs 74%), however this did not reach statistical significance, p>0.05. No significant difference between early AE (9% Vs 10%) or late AE (10% Vs 8%), or in complete resolution of the cyst at 3 months follow up (81% Vs 83%), in patients with and without splanchnic varices, p>0.05 for all. Conclusion Patients with splanchnic varices who undergo EUD for PP have significantly higher intra-procedural complications, as compared to those patients without varices. However, long term outcome measures, in terms of AE and cyst resolution, are comparable between both groups. Disclosure of Interest None Declared
Journal Title: Gut
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!