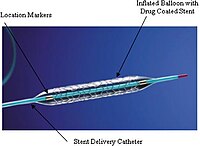
Photo from wikipedia
Objective Therapeutic strategies for atrial septal defect (ASD) with severe pulmonary arterial hypertension (PAH) are controversial. This study aimed to evaluate the efficacy of PAH-specific medications and subsequent transcatheter closure… Click to show full abstract
Objective Therapeutic strategies for atrial septal defect (ASD) with severe pulmonary arterial hypertension (PAH) are controversial. This study aimed to evaluate the efficacy of PAH-specific medications and subsequent transcatheter closure (ie, treat-and-repair strategy) on clinical outcomes. Methods We enrolled 42 patients who were referred to 13 institutions for consideration of ASD closure with concomitant PAH and underwent the treat-and-repair strategy. The endpoint was cardiovascular death or hospitalisation due to heart failure or exacerbated PAH. Results At baseline prior to PAH-specific medications, pulmonary to systemic blood flow ratio (Qp:Qs), pulmonary vascular resistance (PVR), and mean pulmonary artery pressure (PAP) were 1.9±0.8, 6.9±3.2 Wood units and 45±15 mm Hg. Qp:Qs was increased to 2.4±1.2, and PVR and mean PAP were decreased to 4.0±1.5 Wood units and 35±9 mm Hg at the time of transcatheter ASD closure after PAH-specific medications. Transcatheter ASD closure was performed without any complications. During a median follow-up period of 33 months (1–126 months) after transcatheter ASD closure, one older patient died and one patient was hospitalised due to heart failure, but the other patients survived with an improvement in WHO functional class. PAP was further decreased after transcatheter ASD closure. Conclusions The treat-and-repair strategy results in low complication and mortality rates with a reduction in PAP in selected patients with ASD complicated with PAH who have a favourable response of medical therapy.
Journal Title: Heart
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!