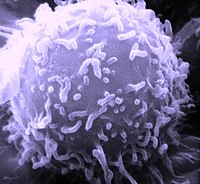
Photo from wikipedia
Immune-related adverse events (irAE) may affect almost any organ system and occur at any point during treatment with immune checkpoint inhibitors (ICI). We present a patient with advanced lung cancer… Click to show full abstract
Immune-related adverse events (irAE) may affect almost any organ system and occur at any point during treatment with immune checkpoint inhibitors (ICI). We present a patient with advanced lung cancer receiving antiprogrammed death 1 checkpoint inhibitor who developed a delayed-onset visual irAE treated with corticosteroids. Through assessment of longitudinal biospecimens, we analyzed serial autoantibodies, cytokines, and cellular populations. Months after ICI initiation and preceding clinical toxicity, the patient developed broad increases in cytokines (most notably interleukin-6 (IL-6), interferon-γ (IFNγ), C-X-C motif chemokine ligand 2 (CXCL2), and C–C motif chemokine ligand 17 (CCL17)), autoantibodies (including anti-angiotensin receptor, α-actin, and amyloid), CD8 T cells, and plasmablasts. Such changes were not observed in healthy controls and ICI-treated patients without irAE. Administration of corticosteroids resulted in immediate and profound decreases in cytokines, autoantibodies, and inflammatory cells. This case highlights the potential for late-onset changes in humoral and cellular immunity in patients receiving ICI. It also demonstrates the biologic effects of corticosteroids on these parameters. Application of humoral and cellular immune biomarkers across ICI populations may inform toxicity monitoring and management.
Journal Title: Journal for Immunotherapy of Cancer
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!