Photo from wikipedia
Background Cancer stem cells (CSC) define a population of rare malignant cells endowed with ‘stemness’ properties, such as self-renewing, multipotency and tumorigenicity. They are responsible for tumor initiation and progression,… Click to show full abstract
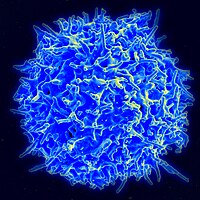
Background Cancer stem cells (CSC) define a population of rare malignant cells endowed with ‘stemness’ properties, such as self-renewing, multipotency and tumorigenicity. They are responsible for tumor initiation and progression, and could be associated with resistance to immunotherapies by negatively regulating antitumor immune response and acquiring molecular features enabling escape from CD8 T-cell immunity. However, the immunological hallmarks of human lung CSC and their potential interactions with resident memory T (TRM) cells within the tumor microenvironment have not been investigated. Methods We generated a non-small cell lung cancer model, including CSC line and clones, and autologous CD8+CD103+ TRM and CD8+CD103− non-TRM clones, to dissect out immune properties of CSC and their susceptibility to specific T-cell-mediated cytotoxic activity. Results Unlike their parental tumor cells, lung CSC are characterized by the initiation of an epithelial-to-mesenchymal transition program defined by upregulation of the SNAIL1 transcription factor and downregulation of phosphorylated-GSK-3β and cell surface E-cadherin. Acquisition of a CSC profile results in partial resistance to TRM-cell-mediated cytotoxicity, which correlates with decreased surface expression of the CD103 ligand E-cadherin and human leukocyte antigen-A2-neoepitope complexes. On the other hand, CSC gained expression of intercellular adhesion molecule (ICAM)-1 and thereby sensitivity to leukocyte function-associated antigen (LFA)-1-dependent non-TRM-cell-mediated killing. Cytotoxicity is inhibited by anti-ICAM-1 and anti-major histocompatibility complex class I neutralizing antibodies further emphasizing the role of LFA-1/ICAM-1 interaction in T-cell receptor-dependent lytic function. Conclusion Our data support the rational design of immunotherapeutic strategies targeting CSC to optimize their responsiveness to local CD8+CD103+ TRM cells for more efficient anticancer treatments.