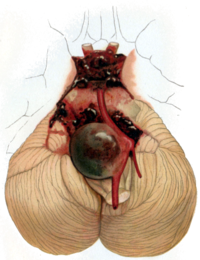
Photo from wikipedia
Background Endovascular treatment of cerebral aneurysms in the posterior circulation poses a challenge because of the higher rate of wide-necked aneurysms and presentation with rupture. In this study, we compare… Click to show full abstract
Background Endovascular treatment of cerebral aneurysms in the posterior circulation poses a challenge because of the higher rate of wide-necked aneurysms and presentation with rupture. In this study, we compare the baseline characteristics and outcomes of patients with posterior circulation aneurysms treated with novel second-generation coils in the SMART registry. Methods SMART is a phase 4, multicenter, prospective, registry that enrolled patients with anterior and posterior circulation cerebral aneurysms (both ruptured and unruptured) who underwent endovascular treatment using Penumbra SMART™ Coils. Collected data included baseline clinical and angiographic characteristics at presentation. Primary and secondary end points were immediate angiographic occlusion, periprocedural complications, recanalization and retreatment rates and mortality at 1-year follow up. We compared the above variables between anterior and posterior circulation aneurysms. Results Of a total of 906 patients treated in the SMART registry, 173 (19.1%) had posterior circulation aneurysms. In comparison to patients with anterior circulation aneurysms, patients with aneurysms in the posterior circulation were older (mean age 61.7 vs. 59.3 years, P 0.017) and more likely to present with rupture (38.7% vs. 30.3%, P 0.032). Posterior circulation aneurysms were more likely to be wide-necked (defined as an aneurysm with a dome-to-neck ratio less than 2.0 and/or a neck length of 4 mm or more). No significant difference was found in the rate of successful embolization at initial procedure (Raymond Class I), serious device-related adverse effects within 24 hours, one-year recanalization and one-year retreatment between both groups (table 1).Abstract O-024 Table 1 Comparison between anterior and posterior circulation aneurysms Baseline characteristics Posterior circulation aneurysm patients (N=173) Anterior circulation aneurysm patients (N=733) P-value Age, Mean SD 61.7 11.6 59.3 12.8 0.017 Female,% (n/N) 78.6% (136/173) 73.9% (542/733) 0.203 Ruptured aneurysm, % (n/N) 38.7% (67/173) 30.3% (222/733) 0.032 Aneurysm Size % (n/N) 0.285 Small (<11mm) 86.1% (149/173) 89.5% (656/733) Large (11 to 25 mm) 13.3% (23/173) 10.4% (76/733) Giant (>25mm) 0.6% (1/173) 0.1% (1/733) Wide-Neck% (n/N) 72.2% (117/162) 59.9% (439/733) 0.002 Stent-Assisted Coiling % (n/N) 38.2% (66/173) 36.2% (265/733) 0.624 Balloon-Assisted Coiling % (n/N) 16.8% (29/173) 20.6% (151/733) 0.255 Raymond Occlusion, Class I Immediate Post-Procedure% (n/N) 37.6% (65/172) 41.1% (298/729) 0.457 One-Year Follow-Up % (n/N) 55.1% (43/78) 64.4% (250/388) 0.121 Recanalization at One-Year Follow-Up % (n/N) 12.8% (10/78) 14% (54/385) 0.205 Retreatment through One-Year Follow-Up 6.2% (5/81) 7% (28/399) 0.190 Device-Related SAE within 24 Hours of Procedure % (n/N) 1.7% (3/173) 3% (22/733) 0.360 Length of Hospital Stay, Median [IQR] 2 [1–14] 1 [1–10] 0.053 Conclusions Despite being associated with higher rates of rupture and wide-necked geometry, patients with posterior circulation aneurysms experienced immediate and one-year angiographic occlusion rates that were not significantly different from anterior circulation aneurysms. Device-related peri-procedural complications were also not significantly higher than the latter. Disclosures E. Almallouhi: None. M. Sattur: None. M. Anadani: None. S. Al kasab: None. A. Spiotta: 2; C; Penumbra, Cerenovus, Minnetronix.
Journal Title: Journal of NeuroInterventional Surgery
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!