Photo from wikipedia
Objective: Bronchial thermoplasty is an effective intervention to improve respiratory symptoms and to reduce the rate of exacerbations in uncontrolled severe asthma. A reduction in airway smooth muscle is arguably… Click to show full abstract
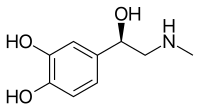
Objective: Bronchial thermoplasty is an effective intervention to improve respiratory symptoms and to reduce the rate of exacerbations in uncontrolled severe asthma. A reduction in airway smooth muscle is arguably the most widely discussed mechanisms accounting for these clinical benefits. Yet, this smooth muscle reduction should also translate into an impaired response to bronchodilator drugs. A pilot study was designed to address this question. Hypothesis: Thermoplasty decreases the response to a bronchodilator. Methods: Lung functions measured by spirometry and respiratory mechanics measured by oscillometry (tremoFlo, Thorasys) were examined pre- and post-bronchodilator (salbutamol, 400 μg) before and after at least 1 year of thermoplasty in 8 patients (7 women) with uncontrolled severe asthma. For each readout, a two-way ANOVA was used to assess the effect of thermoplasty, salbutamol, and their interaction. All procedures were approved by the IUCPQ Ethics Committee. Data: Consistent with previous studies, thermoplasty yielded no benefits in terms of baseline lung function and respiratory mechanics, despite improving symptoms based on two questionnaires assessing the level of asthma control (Asthma Control Questionnaire – ACQ-5, and Asthma Control Test – ACT-5). The response to salbutamol was not affected by thermoplasty based on spirometric readouts, including forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC) and FEV1/FVC ratio. However, a significant interaction was observed between thermoplasty and salbutamol for two oscillometric readouts. The reactance of the respiratory system at 5 Hz (Xrs5) increased from -3.2 ±2.6 to -1.9 ± 1.9 cmH2O ·s/L in response to salbutamol pre-thermoplasty, versus from -2.8 ± 2.3 to -2.2 ± 1.9 cmH2O·s/L post-thermoplasty (interaction, p=0.04). Similarly, the reactance area (Ax) decreased from 32.6 ± 29.0 to 12.8 ±18.2 cmH2O/L in response to salbutamol pre-thermoplasty, versus 27.2 ± 29.4 to 15.7 ± 20.1 cmH2O/L post-thermoplasty (interaction, p=0.02). The salbutamol-induced changes in resistance at 5 Hz (Rrs5), resistance at 19 Hz (Rrs19), Rrs5 minus Rrs19, and resonant frequency were not significantly affected by thermoplasty. Summary of results: While spirometry was unable to detect changes in the response to salbutamol caused by thermoplasty, two oscillometric readouts, namely Xrs5 and Ax, confirmed that the bronchodilator response is attenuated post-thermoplasty. Conclusion: Despite its small size, this study demonstrates that thermoplasty attenuates the response to a bronchodilator. We argue that this result is a physiological proof of therapeutic efficacy, consistent with the well-described effect of thermoplasty in reducing the amount of airway smooth muscle. FQSR (Fondation Quebecoise en Sante Respiratoire); Canadian Institutes of Health Research (PJT-387910); FRQS (Fonds de recherche du Quebec - Sante); and Boston Scientific Inc This is the full abstract presented at the American Physiology Summit 2023 meeting and is only available in HTML format. There are no additional versions or additional content available for this abstract. Physiology was not involved in the peer review process.
Journal Title: Physiology
Year Published: 2023
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!