Photo from wikipedia
Background and Purpose: Delayed cerebral ischemia is a major cause of morbidity and mortality in patients with aneurysmal subarachnoid hemorrhage (aSAH). Cilostazol, a selective inhibitor of phosphodiesterase 3, was reported… Click to show full abstract
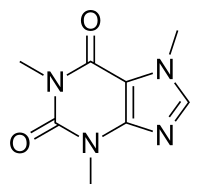
Background and Purpose: Delayed cerebral ischemia is a major cause of morbidity and mortality in patients with aneurysmal subarachnoid hemorrhage (aSAH). Cilostazol, a selective inhibitor of phosphodiesterase 3, was reported to reduce cerebral vasospasm and improve outcomes. We aimed to conduct an updated systematic review and meta-analysis of the efficacy and safety of cilostazol in aSAH. Methods: We systematically searched PubMed, Embase, MEDLINE, and the Cochrane Library for articles published in English with the latest publishing time in August 2020. Articles reporting favorable outcome as the primary outcome and reporting severe angiographic vasospasm (aVS), symptomatic vasospasm (sVS), new cerebral infarction, or mortality as the secondary outcome were included in this review. Furthermore, we examined whether clinical outcomes were associated with the dosage of cilostazol (300 mg/day vs. 100–200 mg/day). Results: Data from 405 patients in 4 randomized controlled trials (RCTs) and 461 patients in 4 observational studies (OSs) were included. In RCT studies, cilostazol was associated with significant favorable outcomes at discharge or 1 month (risk ratio [RR] 1.41, 95% confidence interval [CI] 1.01–1.97, p = 0.04) or 3 or 6 months (RR 1.16, 95% CI 1.05–1.28, p = 0.002). However, in OSs, no significant difference was indicated in favorable outcomes at discharge or 1 month (RR 1.22, 95% CI 0.94–1.60, p = 0.14) nor 3 or 6 months (RR 1.29, 95% CI 0.92–1.81, p = 0.14). The analyses found that cilostazol significantly reduced the incidences of severe aVS (RCT: RR 0.64, 95% CI 0.41–1.01, p = 0.05; OS: RR 0.61, 95% CI 0.43–0.88, p = 0.007), sVS (RCT: RR 0.46, 95% CI 0.31–0.70, p = 0.0002; OS: RR 0.38, 95% CI 0.21–0.68, p = 0.001), and new cerebral infarction (RCT: RR 0.40, 95% CI 0.24–0.67, p = 0.0005; OS: RR 0.38, 95% CI 0.23–0.64, p = 0.0002). However, no significant difference in mortality (RCT: RR 0.86, 95% CI 0.23–3.21, p = 0.82; OS: RR 0.16, 95% CI 0.02–1.24, p = 0.08) was found. In 3 OSs which reported different doses of cilostazol (300 mg/day vs. 100–200 mg/day) for aSAH, the 300-mg/day cilostazol groups showed decreased delayed cerebral infarction (RR 0.27, 95% CI 0.09–0.81, p = 0.02) but no significant difference in shunt-dependent hydrocephalus (RR 0.92, 95% CI 0.33–2.60, p = 0.88) or functional outcomes (RR 1.14, 95% CI 0.74–1.75, p = 0.56) compared with the 100–200 mg/day cilostazol groups. Conclusions: The meta-analyses suggest the credible efficacy and safety of cilostazol in treating aSAH. Furthermore, 300-mg/day cilostazol treatment appeared to be more effective than 100–200 mg/day treatment.
Journal Title: Cerebrovascular Diseases
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!