Photo from wikipedia
In the current issue of Hypertension, Omata et al have made a ground-breaking contribution to our understanding of the genesis of primary aldosteronism (PA). First, however, the background. For many… Click to show full abstract
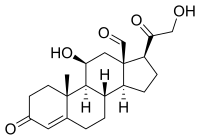
In the current issue of Hypertension, Omata et al have made a ground-breaking contribution to our understanding of the genesis of primary aldosteronism (PA). First, however, the background. For many years the pathogenesis of PA, both unilateral aldosterone-producing adenoma (APA) and (presumedly) bilateral adrenal hyperplasia (now perhaps better termed idiopathic hyperaldosteronism, IHA), remained to be determined. For APA, this changed in 2011, with the finding of somatic mutations in the gene encoding KCNJ5, a component of the Kir 3.4 potassium channel, in 8 out of 22 APA (6 L168R, 2 G151R). This was confirmed and extended in short order by a much larger study from the ENS@T coalition in Europe on 380 APA, demonstrating the same percentage of mutations, younger age, and higher frequency in women— but more G151R than L168R and no difference in APA size, in contrast with the original report. Although KCNJ5 mutations account for 30% to 40% of APA (more in many reports from Japan and China), subsequently a series of less common somatic gain-of-function mutations have been documented. These encode the cation calcium channels (CACNA1D, CACNA1H) and the chloride channel (CLCN2), as well as the K channel KCNJ5, as noted above; they also encode the sodium (ATP1A1) and calcium (ATP2B3) ATPases. Until recently, no equivalent clarity existed for IHA. Key to unlocking the enigma followed the demonstration of adrenal producing cell clusters (APCC) in many (but not all) normal adrenal glands from autopsy specimens in the United States and Japan. In the first study, on 45 normal adrenals from kidney donors, APCCs were identified in approximately half; 8 out of 23 APCCs harboured known aldosterone driver mutations (CACNA1D 6; ATP1A1 2). The second study, on autopsy material from 107 similarly normotensive subjects, showed APCCs in 61 out of 107; of 21 out of 61 harboring somatic mutations, the distribution was similar to that in the first study (16 CACNA1D, 3 ATP2B3, 2 ATP1A1). In addition to the CACNA1D predominance, the second study also showed a clear age-associated increase in APCC score. What Omata et al have done in the present study takes the potential role of APCC in IHA a crucial step further. The previous studies were on patients who were normotensive despite (albeit in a minority of cases) their APPC expressing somatic mutations in known aldosterone driver genes. The step further is to move the stage from normotension to hypertension by the examination of APCC frequency and mutation prevalence in the (very rare) cases of 1 adrenal being removed, despite no indication of lateralization on imaging or adrenal venous sampling. The rationale for this last resort was commonly severe and resistant hypertension and, on occasion, intolerance of conventional medical therapy of IHA; what, if anything, guided the choice of which adrenal was removed in most cases is not clear. Of the 15 initial adrenals, 8 were from Sendai and 7 from Brisbane; one of the latter failed quality assurance so that the results on 14 patients are recorded. The data are electrifying, in 4 ways. First, a total of 99 APCCs were found in the 14 patients, all of whom had at least 1 affected APCC. Second, of the 99 APCCs, 58 harbored a somatic mutation: both these findings contrast starkly with the data on normotensive patients. Third, of the 58 mutations, all but one was in CACNA1D, with 1 in KCNJ5. One of the salient features of APCC is that there is no previously reported case of KCNJ5 expression: this patient had 4 (all mutant) APCCs; the authors' plausible explanation of the G151R KCNJ5 mutation is that it represents a microadenoma. Finally, the authors report an astonishing 26 different mutations in CACNA1D, of which 18 have not been previously reported in sporadic APA, and of which all but one (F1248L) occur only once across the cohort. The authors appropriately conclude that their results support increased autonomous aldosterone production driven by somatic mutations in aldosterone-regulating genes in APCC (nearly exclusively CACNA1D) as the underlying cellular and molecular pathobiology of IHA. Coupled with previous studies in APA and computed tomography-negative unilateral PA, their findings in IHA suggests that the majority of PA results from somatic mutations in aldosterone-regulating genes that influence intracellular calcium homeostasis. Importantly, as opposed to APA, computed tomography-negative PA is primarily caused by mutations in CACNA1D. Voltage-dependent calcium channels, such as CACNA1D mediate the entry of Ca into excitable cells; they are multisubunit complexes comprising α-1, β, α-2/δ, and γ subunits. Channel activity is directed by the poreforming α-1 subunits, with the others regulating this activity. The different properties of the calcium channel subtypes The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association. From the Hudson Institute of Medical Research and Monash University, Victoria, Australia. Correspondence to John W Funder, Hudson Institute of Medical Research, Steroid Biology, Block E, 246 Clayton Rd, Clayton, Victoria 3168, Australia. Email [email protected] Idiopathic Hyperaldosteronism New Answers, New Questions
Journal Title: Hypertension
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!