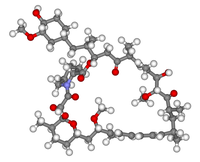
Photo from wikipedia
Cellular signaling controlled by the serine/threonine kinase mTOR regulates, via the two complexes mTORC1 and mTORC2, fundamental cell functions such as organismal growth, proliferation, autophagy, aging, survival, and metabolism (1).… Click to show full abstract
Cellular signaling controlled by the serine/threonine kinase mTOR regulates, via the two complexes mTORC1 and mTORC2, fundamental cell functions such as organismal growth, proliferation, autophagy, aging, survival, and metabolism (1). It is therefore not surprising that mTOR inhibitors (mTORi) are increasingly used clinically, primarily as immunosuppressants and oncotherapeutics, for the management of multiple conditions, including lung transplantation and lymphangioleiomyomatosis. U.S. Food and Drug Administration-approved in 1997 as treatment for organ transplant allograft rejection, the first generation of mTORi include rapamycin and its analogs (rapalogs) that target mTORC1. The more potent second generation of inhibitors, that target both mTORC1 and mTORC2 are being evaluated in clinical trials and little is known about their risk profile. In turn, the side effects of rapalogs are better characterized. These include stomatitis, hyperglycemia, hyperlipidemia, increased risk for infections, and noninfectious pneumonitis (2). Although variable in severity and often responsive to drug dose reduction or corticosteroid therapy, noninfectious pneumonitis complicates the clinical management of patients requiring rapalog treatment (3, 4). Characterized histologically by lymphocytic interstitial infiltrates (4), the pathogenesis of lung injury caused by rapalogs is not yet elucidated. In this issue of the Journal, the work by Chen and colleagues (pp. 646–657) provides new insight into the mechanisms that may underlie the development of lung inflammation in response to mTORi, focusing on the role of the dual mTORC1 and mTORC2 inhibition in the lung endothelium as a key point of vulnerability (5). Building on their previous report that rapalogs augment endotoxin (LPS)-induced pulmonary edema (6), Chen and colleagues use mice with conditional endothelial cell–specific deletion ofMtor, Rptor, or Rictor to solidify the importance of mTOR in maintaining the barrier function of the endothelium. In particular, they show that mice with (haplo) insufficient vascular mTORC1 or mTORC2 function are more vulnerable to acute lung injury, as they develop marked hyperpermeability and inflammation upon LPS inhalation. Their complementary studies in human umbilical vein endothelial cells (ECs) with confirmatory studies in an simian virus 40 transformed human lung EC line show that either mTORC1 or mTORC1 and 2 inhibition with rapamycin or torin 1, respectively, promote EC contraction and hyperpermeability. Indeed, by using mTORi as well as knockdown of Raptor, Rictor, and mTOR, these investigators, for the first time, link mTORC1 and mTORC2 with cascades of kinase activation that culminate in increased myosin light chain phosphorylation and endothelial cytoskeletal contraction, increased intercellular gaps, and increased endothelial monolayer permeability. They implicate that mTORi stimulate both PKCa and PKCd, with respective downstream activation of Rho-associated kinase and of myosin light chain kinase transcription by p38 and NFkB. It is noteworthy that no phenotypic changes were noted in adult mice with haploid or conditional diploid depletion of endothelial Rptor or Rictor at baseline, whereas diploid loss of these genes in the endothelium during development is embryonically lethal (7). Although the subpotent efficiency of the target deletion ( 50%) could explain these results, it is also possible that the effect of mTORi in the adult endothelium, during quiescent homeostatic conditions with low metabolic and repair demands, is better tolerated in mice. However, the findings that the inhibition of mTOR in ECs is sufficient to increase the vulnerability of mice to a more severe lung injury from a second hit such as LPS may be relevant to understanding the pulmonary toxicity from mTORi. Because exposures to LPS, for example, via gram-negative bacterial respiratory infections or sepsis or even from repetitive cigarette smoke inhalation, are not uncommon in patients undergoing organ transplantation or suffering from cancer, treatment with mTORi could increase their risk for acute lung injury. Indeed, one of the more potent endogenous mTORi, Rtp801, a protein sensor that is activated by stresses such as hypoxia and cigarette smoking, significantly augments the degree of lung injury and inflammation induced by LPS (8, 9). Although these and the current findings by Chen and colleagues provide compelling evidence that the mTORi-induced lung injury phenotype requires a “double-hit” event, further mechanistic research and analysis of clinical safety data are needed to determine if the endothelial inhibition of mTOR by rapalogs is necessary to cause lung toxicity or to enhance the risk of lung injury in patients. Although the study by Chen and colleagues refines our understanding of the role of the endothelium in promoting lung inflammation in response to mTORi, we would be remiss in not acknowledging that the models used here might not fully reflect the pathophysiological processes in human subjects. For example, as the authors acknowledge, the mouse model did not exhibit lymphocytic interstitial pneumonitis characteristic of lung toxicity caused by rapalogs, and the levels of mTORi studied here may not reflect those used clinically. Furthermore, it remains to be demonstrated if a reconstitution of mTOR function in the endotheliumwould prevent the pulmonary toxicity of the broad multicellular mTOR inhibition achieved by pharmacotherapy. Future validation of the findings of the current report could support
Journal Title: American Journal of Respiratory Cell and Molecular Biology
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!