Photo from wikipedia
Neuromuscular diseases (NMD) are indications for long-term home mechanical ventilation (HMV). Noninvasive ventilation is preferred to HMV. However, invasive mechanical ventilation (IMV) is more appropriate if the patient has uncontrollable… Click to show full abstract
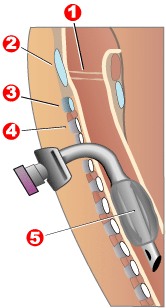
Neuromuscular diseases (NMD) are indications for long-term home mechanical ventilation (HMV). Noninvasive ventilation is preferred to HMV. However, invasive mechanical ventilation (IMV) is more appropriate if the patient has uncontrollable airway secretions, the possibility of aspiration, failure to wean, or severe weakness of the respiratory muscles. But if the patient undergoes multiple intubation or tracheotomy, it will be more painful and unbearable. For some end-stage NMD patients who need long-term tracheostomy, HMV using noninvasive ventilator via tracheotomy may be a conservative care option. An 87-year-old male with myasthenia gravis underwent repeated IMV and failed to wean. We used a noninvasive ventilator connected to a tracheostomy tube for mechanical ventilation. One and a half years later, the patient weaned successfully. However, there was a lack of evidence-based medicine and standardized guidelines in such areas as indications, contraindications, and ventilator parameter setting. For the systematic review, a literature search was performed in PubMed, Embase, Cochrane, and CNKI (China National Knowledge Infrastructure) to identify reported cases of using noninvasive ventilator in patients undergoing tracheostomy. A total of 72 cases who performed ventilation via tracheotomy tube were identified. The main diagnoses included NMD, chronic obstructive pulmonary disease (COPD), pneumonia, and congenital central hypoventilation syndrome (CCHS). Indications included dysfunctional ventilatory weaning response (DVWR), apnea and cyanosis. Clinical outcome was as follows: 33 patients were weaned, and 24 patients underwent HMV. A total of 288 cases who performed ventilation through the mask after blocking the tracheostomy tube were identified. The primary diagnoses included COPD, NMD, thoracic restriction, spinal cord injured (SCI), and CCHS. Indications included DVWR, apnea and cyanosis, routine weaning. Clinical outcome was as follows: successful tracheostomy tube decannulations were performed in 254 patients and failed in 33 patients. So, in patients requiring HMV, selection of noninvasive ventilation (NIV) or IMV should be individualized. Tracheostomy preservation should be considered in some patients with advanced NMD if there is respiratory muscle weakness or the risk of aspiration. And attempts can be made to use a noninvasive ventilator because of its advantages of portability, ease of operation, and low cost. Noninvasive ventilators can be used in patients with tracheotomy, whether direct connection tracheotomy or mask ventilation after the tube is capped, especially in weaning and tracheostomy tube decannulation.
Journal Title: Therapeutic Advances in Respiratory Disease
Year Published: 2023
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!