Photo from wikipedia
We present the case of a 56-year-old woman who was diagnosed with severe coronavirus disease 2019 (COVID-19) pneumonia complicated by severe acute respiratory distress syndrome who was intubated for 19… Click to show full abstract
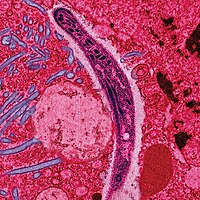
We present the case of a 56-year-old woman who was diagnosed with severe coronavirus disease 2019 (COVID-19) pneumonia complicated by severe acute respiratory distress syndrome who was intubated for 19 days. She recovered from COVID-19 after a month. A computed tomography (CT) scan of the chest, after a month, showed improved infiltrates with a small residual cavity within the lingula. A CT angiogram showed a more confluent density in the lingular portion on follow-up 2 months later. She developed intermittent hemoptysis after 3 months in December 2020, which persisted for almost 6 months, and CT of the chest showed the lingular nodular with resolution of the cavitation. She underwent bronchoscopy with bronchoalveolar lavage, confirming Aspergillus fumigatus by galactomannan assay and histology showing branching hyphae. Once she started treatment with itraconazole, her hemoptysis resolved. The follow-up CT of the chest after 2 months of treatment did not show a cavity or a nodule in the lingula. Our patient developed invasive pulmonary aspergillosis (IPA) as a sequela of severe COVID-19 infection. COVID-19-associated invasive pulmonary aspergillosis (CAPA) is an underrecognized complication that needs to be investigated on whether prophylactic treatment is required. Our case also demonstrates that the diagnosis of IPA needs to be considered months after COVID-19 infection when a superimposed fungal infection can occur after a viral infection if the patient continues to have persistent symptoms.
Journal Title: Journal of Investigative Medicine High Impact Case Reports
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!