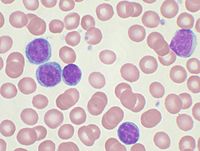
Photo from wikipedia
Background. Non-chronic lymphocytic leukemia (non-CLL) clonal B-cell lymphocytosis (CBL) encompasses a heterogeneous group of hematologic disorders that are still poorly understood. The main purpose of this study was to explore… Click to show full abstract
Background. Non-chronic lymphocytic leukemia (non-CLL) clonal B-cell lymphocytosis (CBL) encompasses a heterogeneous group of hematologic disorders that are still poorly understood. The main purpose of this study was to explore the genomic landscape of non-CLL CBL, correlating the results with clinical, histological and immunogenetic features. Methods. We retrospectively analysed the disease characteristics in a highly selected series of 28 patients, who had a clonal lymphocytosis in peripheral blood (PB) and clonal lymphoid populations in the bone marrow (BM), without evidence of lymphadenopathy, splenomegaly, peripheral cytopenia or constitutional symptoms.In all patients the BM evaluation, comprising flow cytometry, histology and immunohistochemistry, was not able to classify the lymphoproliferative disorder in any of the WHO-defined entities. A diagnosis of CLL or a leukemic phase of mantle cell or follicular lymphoma was ruled out in each subject. Targeted next generation sequencing (NGS) was performed on DNA extracted from CD19+ BM or PB cells using a core panel of 138 genes frequently reported in mature B cell neoplasms.On the basis of the information retrieved from the KEGG and REACTOME databases, each mutated gene was assigned to a specific lymphoma-enriched pathway. Results: Clinical, flow cytometric and histological data are presented in Table 1.The median BM infiltration was 30% (range: 5-80%); the pattern of infiltration was interstitial or mixed (nodular and interstitial) in the majority of the cases; sinusoidal localization was noticed in 54% of cases. There was a borderline correlation between the extent of BM infiltration and the absolute number of PB clonal B cells count (Spearman's Rho: 0.38, p=0.05), that ranged from 851/mmc to 14508/mmc (median: 3604/mmc). With a median follow-up of 35.2 months (range: 6-125), only 1 patient developed disease progression to a B-cell lymphoma not otherwise specified (5-yrs CI of progression: 11.9%; 95%CI: 0.6%-40.7%). The sequence analysis of 138 genes revealed a total number of 74 somatic mutations in 51 genes. All the 28 cases displayed at least 1 mutation, with the number of mutations ranging from 1 to 7 (median 2). The most frequently mutated genes were MYD88 (14%), PDE4DIP (14%), BIRC3 (11%), CCND3 (11%), NOTCH1 (11%) and TNFAIP3 (11%) (fig.1).Notably, 3 out of 4 MYD88 variants were different from the classical p.L265P (p.M232T, p.V217F and p.L204F not previously described). Data on IGHV were available for 22 patients (79%) (Fig.2): VH gene repertoire was similar to that reported in non-CLL malignancies and no distinct stereotyped subset was found. Truly unmutated IGHV genes with 100% of germline identity were present in 3 cases (11%). The analysis of disease features according to mutated genes showed that MCwas more frequent in patients harbouring mutations in MYD88 (p=0.08) or TNFAIP3 (p=0.02); these patients had also a higher number of mast cells on BM histology than the wild type ones (p=0.02 and p=0.05, respectively). NOTCH1 mutated patients showed an absolute number of B-cell peripheral clonal lymphocytes higher than wild type cases (p=0.037). The most frequently involved pathways were NF-kB signalling (32%) and cell communication pathways (32%), followed by cell cycle (29%), chromatin organization (25%), transcriptional misregulation (21%), Toll-like receptor (TLR) signalling (18%) and NOTCH signalling pathways (14%) (Fig. 3).Patients with mutated chromatin organization pathway more often showed normal LDH levels compared with wild type cases (100% vs 40% p=0.01). Conclusions. We characterised non-CLL CBL, integrating BM histological features and IGHV data with an extended NGS panel. The mutational landscape was extremely heterogeneous, pointing out a wide spectrum of somatic mutations. Most of them have been already described in Waldenström's Macroglobulinemia and splenic B-cell lymphomas; of note, we found a new variant of MYD88 associated with an IgM MC and recurrent mutations of PDE4DIP, which have not been previously reported in indolent B-cell malignancies. Varettoni: Janssen: Consultancy; Roche: Consultancy; ABBVIE: Other: travel expenses; Gilead: Other: travel expenses. Arcaini:Bayer, Celgene, Gilead Sciences, Roche, Sandoz, Janssen-Cilag, VERASTEM: Consultancy; Celgene: Speakers Bureau; Celgene, Roche, Janssen-Cilag, Gilead: Other: Travel expenses; Gilead Sciences: Research Funding.
Journal Title: Blood
Year Published: 2019
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!