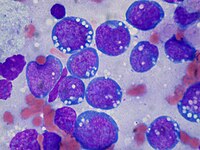
Photo from wikipedia
e18655 Background: Dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin DA-(EPOCH)-containing regimens are frequently utilized in lymphoma, however, outpatient EPOCH or modified inpatient/outpatient EPOCH has not been described extensively. We transitioned inpatient… Click to show full abstract
e18655 Background: Dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin DA-(EPOCH)-containing regimens are frequently utilized in lymphoma, however, outpatient EPOCH or modified inpatient/outpatient EPOCH has not been described extensively. We transitioned inpatient EPOCH to the outpatient setting and modified EPOCH to be given in the inpatient setting with rituximab outpatient to improve quality of care and access to patient assistance programs. Methods: A single-center, institutional review board-approved retrospective study was conducted for adults receiving EPOCH-based regimens. Data were collected by chart review for each patient between January 2013 and September 2020. The primary outcomes were to determine the incidence of chemotherapy delays due to disease-related reasons as febrile neutropenia (FN), adverse events or abnormal labs and the incidence of FN between patients receiving inpatient (IP), outpatient (OP), or combination inpatient/outpatient DA-EPOCH +/- R (hybrid). Secondary cost analysis including hospital stay cost, chemotherapy and laboratory monitoring costs was performed for the three settings. Results: A total of 43 patients received 175 cycles of an EPOCH regimen (18 [10.3%] IP), 90 [51.4%] OP, and 67 [38.3%] hybrid). The mean maximum dose level achieved with DA-EPOCH+/-R was dose level 2 with the average number of cycles at 4.1 cycles/patient. A total of 15 cycles were delayed due to disease related reasons: 1 (6%) in IP, 12 (18%) in hybrid (P = 0.196, when compared with IP) and 2 (2%) in OP (P = 0.432 when compared with IP). A total of 166 cycles received granulocyte-colony stimulating factor (G-CSF); 16 cycles (9.6%) administered IP with a FN incidence of two (12.5%), 62 cycles (37.4%) administered in the hybrid setting with a FN incidence of seven (11.3%) (P = 0.893 when compared with IP) and 88 cycles (53%) administered OP with a FN incidence of ten (11.3%) (P = 0.896 when compared with IP). The incidence of FN was 9.3% and 12.7% in patients received pegfilgrastim same day versus next day, respectively, P = 0.558. The incidence of FN in patients received reference pegfilgrastim was 9.5% vs 7.7% for patients received pegfilgrastim-cbqv in OP setting (P = 1.00). Transitioning EPOCH to a hybrid IP/OP or OP setting yielded a total cost savings to the health-system of $3,523,174 with 607 hospital bed days saved. Conclusions: EPOCH-containing regimens can be safely transitioned into the outpatient setting or utilized as a hybrid of EPCOH and outpatient Rituximab after chemotherapy side effects can be monitored and outcomes optimized, to better adapt treatment strategies for individualized patient therapies. As new healthcare payment models are developed, outpatient treatments allow for adaptive financial options both for the payor and the patient.
Journal Title: Journal of Clinical Oncology
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!