Photo from wikipedia
Abstract Background: Iodine is essential for the formation of thyroid hormones. Therefore, the thyroid gland is generally able to maintain normal hormone synthesis despite changes in iodine availability. When there… Click to show full abstract
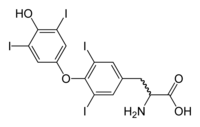
Abstract Background: Iodine is essential for the formation of thyroid hormones. Therefore, the thyroid gland is generally able to maintain normal hormone synthesis despite changes in iodine availability. When there is an increase in iodide load, the thyroid gland is able to inhibit the formation of organic iodide via the Wolff-Chaikoff effect (WCE). This prevents the formation of large quantities of thyroid hormones, thus preventing hyperthyroidism1. Continued exposure to excess iodine is also overcome by the “escape” phenomenon and hormone synthesis resumes in a normal fashion2. However, some patients may lack this autoregulation and develop hypothyroidism. Clinical Case: An 86-year-old male with a history of subclinical hypothyroidism initially presented to his PCP for evaluation of cognitive decline. Workup revealed a TSH of 10 mcIU/mL (0.34 – 5.6 mcIU/mL), a normal FT4 and a negative TPOAb. It was subsequently revealed that the patient was started on Iodoral 12.5 mg daily, an iodine/potassium iodide supplement, 1 month prior to presentation by a naturopathic doctor. Prior to all this, his TSH had always ranged between 4 – 6 mcIU/mL for many years. It was recommended that he discontinue Iodoral and repeat thyroid labs in the future. Despite this, the patient continued on varying doses of Iodoral supplementation. Repeat labs obtained 8 months later revealed an elevated TSH of 99 mcIU/mL and a low FT4 of 0.43 ng/mL (0.6 – 2.6 ng/mL). Despite these numbers, he was asymptomatic and did not exhibit any overt signs of hypothyroidism. He was referred to Endocrinology and finally stopped taking Iodoral.7 weeks post-discontinuation, his repeat labs showed a resolution of hypothyroidism and return to his baseline subclinical disease with a TSH of 8.2 mcIU/mL and a normal FT4. A urine iodine/creatinine was normal at 244.2 ug/g (35 – 540 ug/g) indicating that there was no residual iodine excess from the Iodoral. Conclusion: As far as we are aware, we present the first reported case of Iodoral-induced iatrogenic hypothyroidism. As with past cases of iodine-induced hypothyroidism, our patient had underlying thyroid disease in subclinical hypothyroidism which could explain why he was unable to escape from the WCE. The half-life of Iodoral is unknown but it is generally understood that the effects of iodide are reversed between 2 to 4 weeks after withdrawal. Our patient did not repeat his thyroid function tests until 7 weeks post-discontinuation but did demonstrate a return to baseline with no other intervention. Reference: 1. Markou K, Georgopoulos N, Kyriazopoulou V, Vagenakis AG. Iodine-Induced hypothyroidism. Thyroid. 2001 May;11(5):501-10. doi: 10.1089/105072501300176462. PMID: 11396709.2. Torti JF, Correa R. Potassium Iodide. 2020 Oct 12. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–. PMID: 31194460.
Journal Title: Journal of the Endocrine Society
Year Published: 2021
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!