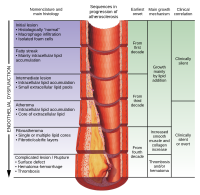
Photo from wikipedia
BACKGROUND AND OBJECTIVES In pooled analyses of endarterectomy trials for symptomatic carotid stenosis, several subgroups experienced no net benefit from revascularization. The validated SCAIL score includes stenosis severity and inflammation… Click to show full abstract
BACKGROUND AND OBJECTIVES In pooled analyses of endarterectomy trials for symptomatic carotid stenosis, several subgroups experienced no net benefit from revascularization. The validated SCAIL score includes stenosis severity and inflammation measured by Positron-Emission Tomography (PET) and improves the identification of patients with recurrent stroke compared with lumen-stenosis alone. We investigated if the SCAIL score improves the identification of recurrent stroke in subgroups with uncertain benefit from revascularization in endarterectomy trials. METHODS We did an individual-participant data pooled analysis of three prospective cohort studies (DUCASS, 2008-2011; BIOVASC, 2014-2018; Barcelona Plaque Study, 2015-2018). Eligible patients had a recent non-severe (modified Rankin Score≤3) anterior circulation ischaemic stroke/TIA and either: ipsilateral mild carotid stenosis (<50%); ipsilateral moderate carotid stenosis (50-69%) plus at least one of female sex, age <65 years, diabetes mellitus, TIA, or delay >14 days to revascularization; or monocular loss of vision. Patients underwent co-registered carotid 18F-FDG PET/CT angiography (≤7 days from inclusion). The primary outcome was 90-day ipsilateral ischaemic stroke. Multivariable Cox regression modelling was performed. RESULTS We included 135 patients. All patients started optimal modern-era medical treatment at admission and 62 (45.9%) underwent carotid revascularization (36 within the first 14 days and 26 beyond). At 90 days, 18 (13.3%) patients had experienced at least one stroke recurrence. The risk of recurrence increased progressively according to the SCAIL score (0.0% in patients scoring 0-1, 15.1% scoring 2-3 and 26.7% scoring 4-5; p=0.04). The adjusted (age, smoking, hypertension, diabetes mellitus, carotid revascularization, antiplatelets and statins) Hazard Ratio for ipsilateral recurrent stroke per 1-point SCAIL increase was 2.16 (95% CI 1.32-3.53; p=0.002). A score ≥2 had a sensitivity of 100% for recurrence. DISCUSSION The SCAIL score improved the identification of early recurrent stroke in subgroups that did not experience benefit in endarterectomy trials. Randomized trials are needed to test if a combined stenosis-inflammation strategy will improve selection for carotid revascularization where benefit is currently uncertain. CLASSIFICATION OF EVIDENCE This study provides Class II evidence that in patients with recent anterior circulation ischemic stroke who do not benefit from carotid revascularization, the SCAIL score accurately distinguishes those at risk for recurrent ipsilateral ischemic stroke.
Journal Title: Neurology
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!