Photo from wikipedia
Bangladesh, a South Asian country with over 165 million people, is currently confronting the worst phase of the Coronavirus Disease 2019 (COVIDAU : PleasenotethatCOVID 19hasbeendefinedasCoronavirusDisease2019atitsfirstmentioninthesentenceBangladesh; aSouthAsiancountrywithover165millionpeople:::Pleasecorrectifnecessary: -19) pandemic since the… Click to show full abstract
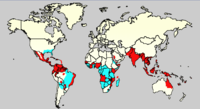
Bangladesh, a South Asian country with over 165 million people, is currently confronting the worst phase of the Coronavirus Disease 2019 (COVIDAU : PleasenotethatCOVID 19hasbeendefinedasCoronavirusDisease2019atitsfirstmentioninthesentenceBangladesh; aSouthAsiancountrywithover165millionpeople:::Pleasecorrectifnecessary: -19) pandemic since the official declaration on 8 March 2020, with a record surge in cases and deaths. After ravaging the neighboring countries (India and Nepal), the highly contagious delta variant has been spreading rapidly throughout Bangladesh. While more than 110,000 confirmed cases and 17,894 deaths had been reported in Bangladesh as of 19 July 2021, the ongoing third wave (MayAU : PleasecheckandconfirmthattheeditstothedatesinthesentenceWhilemorethan110; 000confirmedcasesand17; 894:::arecorrect; andamendifnecessary: to 1 Ju y 2021) has already affected over 300,000 and claimed more than 6,000 lives [1]. However, this is merely an underrepresentation of the actual scenario due to a low level of testing in Bangladesh [2]. To contain the infection, a nationwide lockdown (limited office openings and transport services) has been imposed since 5 April 2021. Later, the government has deployed the military to implement the strictest version of lockdown (all offices and transports were closed) from 1 July 2021. However, the onslaught of this wave is yet to show any sign of slowing down. It is important to mention here that unlike in developed countries, lockdowns were not practically implemented in Bangladesh because of poor general health awareness, public reluctance, and other socioeconomic factors. As a result, almost all hospital beds dedicated to severe and critical patient care in the country, especially those in Dhaka, are currently occupied by patients of COVID-19 [3]. On the other hand, the country’s vaccine drive is still at an early stage; only around 3% (as of 19 July 2021) of the country’s population has received 2 doses. Now vaccination coverage has reached to 20.32% as of 24 November 2021 [4]. Bangladesh is also a hyperendemic country for dengue infection [5]. In recent years, Bangladesh witnessed an upsurge of vector-borne disease outbreaks in Dhaka city, especially dengue and chikungunya. The first-ever massive outbreak of chikungunya in 2017 was followed by the largest outbreak of dengue in 2019 [6,7]. While dengue was causing small outbreaks in every few years since its first appearance in 2000, the 2019 outbreak broke all records and caused the hospitalization of more than 100,000 dengue patients, affecting every age group and socioeconomic stratum [7]. The healthcare system almost collapsed, causing widespread panic in the city. Unfortunately, dengue outbreaks are expected in Dhaka city during every monsoon season because of the high population density, unplanned urbanization, and favorable climatic conditions for vectors [8,9]. Given the current context of the COVID-19 pandemic, a concurrent dengue outbreak is expected to bring catastrophe. This concurrent outbreak in a resource-constraint country is likely to be a unique event. Therefore, experiences from these simultaneous outbreaks would be vital for managing future infectious disease outbreaks elsewhere in the world. PLOS NEGLECTED TROPICAL DISEASES
Journal Title: PLoS Neglected Tropical Diseases
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!