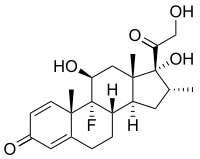
Photo from wikipedia
Antenatal corticosteroids administered to the mother prior to birth decrease the risk of mortality and major morbidity in infants born at less than 35 weeks’ gestation. However, the evidence relating… Click to show full abstract
Antenatal corticosteroids administered to the mother prior to birth decrease the risk of mortality and major morbidity in infants born at less than 35 weeks’ gestation. However, the evidence relating to women with diabetes in pregnancy is limited. Clinical guidelines for antenatal corticosteroid administration recommend that women with diabetes in pregnancy are treated in the same way as women without diabetes, but there are no recent descriptions of whether contemporary practice complies with this guidance. This study is a retrospective review of antenatal corticosteroid administration at a New Zealand tertiary hospital in women with diabetes in pregnancy. We found that in this cohort, for both an initial course at less than 35 weeks’ gestation and repeat courses at less than 33 weeks’, the administration of antenatal corticosteroid to women with diabetes in pregnancy is largely consistent with current Australian and New Zealand recommendations. However, almost 25% of women received their last dose of antenatal corticosteroid at or beyond the latest recommended gestation of 35 weeks’ gestation. Pre-existing diabetes and planned caesarean section were independently associated with an increased rate of antenatal corticosteroid administration. We conclude that diabetes in pregnancy does not appear to be a deterrent to antenatal corticosteroid administration. The high rates of administration at gestations beyond recommendations, despite the lack of evidence of benefit in this group of women, highlights the need for further research into the risks and benefits of antenatal corticosteroid administration to women with diabetes in pregnancy, particularly in the late preterm and early term periods.
Journal Title: PLoS ONE
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!