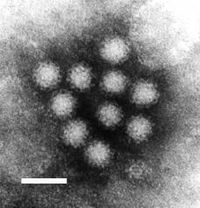
Photo from wikipedia
Background Lymphatic filariasis (LF) is widely endemic in Côte d’Ivoire, and elimination as public health problem (EPHP) is based on annual mass drug administration (MDA) using ivermectin and albendazole. To… Click to show full abstract
Background Lymphatic filariasis (LF) is widely endemic in Côte d’Ivoire, and elimination as public health problem (EPHP) is based on annual mass drug administration (MDA) using ivermectin and albendazole. To guide EPHP efforts, we evaluated Wuchereria bancrofti infection indices among humans, and mosquito vectors after four rounds of MDA in four cross-border health districts of Côte d’Ivoire. Methodology We monitored people and mosquitoes for W. bancrofti infections in the cross-border health districts of Aboisso, Bloléquin, Odienné and Ouangolodougou, Côte d’Ivoire. W. bancrofti circulating filarial antigen (CFA) was identified using filariasis test strips, and antigen-positive individuals were screened for microfilaremia. Moreover, filarial mosquito vectors were sampled using window exit traps and pyrethrum sprays, and identified morphologically at species level. Anopheles gambiae s.l. and Culex quinquefasciatus females were analyzed for W. bancrofti infection using polymerase chain reaction (PCR) technique. Principal findings Overall, we found a substantial decline in W. bancrofti infection indices after four rounds of MDA compared to pre-MDA baseline data. CFA prevalence fell from 3.38–5.50% during pre-MDA to 0.00–1.53% after MDA interventions. No subjects had detectable levels of CFA in Ouangolodougou. Moreover, post-MDA CFA prevalence was very low, and below the 1% elimination threshold in Aboisso (0.19%) and Odienné (0.49%). Conversely, CFA prevalence remained above 1% in Bloléquin (1.53%). W. bancrofti microfilariae (Mf) were not found in Aboisso, Bloléquin, and Ouangolodougou, except for Odienné with low prevalence (0.16%; n = 613) and microfilaremia of 32.0 Mf/mL. No An. gambiae s.l. and Cx. quinquefasciatus pools were infected with W. bancrofti in Bloléquin and Ouangolodougou, while they exhibited low infection rates in Aboisso (1% and 0.07%), and Odienné (0.08% and 0.08%), respectively. Conclusions In cross-border areas of Côte d’Ivoire, LF infection indices in humans and mosquito vectors substantially declined after four rounds of MDA. CFA prevalence fell under the World Health Organization (WHO)-established threshold (1%) in Aboisso, Ouangolodougou and Odienné. Moreover, W. bancrofti prevalence in mosquitoes was lower than WHO-established threshold (2%) in all areas. This might suggest the interruption of W. bancrofti transmission, and possible MDA cessation. However, a formal transmission assessment survey (TAS) and molecular xenomonitoring in mosquito vectors should be implemented before eventual MDA cessation. However, MDA should pursue in Bloléquin where W. bancrofti infection prevalence remained above 1%. Our results provided important ramifications for LF control efforts towards EPHP in Côte d’Ivoire.
Journal Title: PLoS ONE
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!