Photo from wikipedia
We read the article entitled ‘‘Short-term outcome of acute inferior wall myocardial infarction (IWMI) with emphasis on conduction blocks: a prospective observational study in Indian population’’ by Kumar et al.… Click to show full abstract
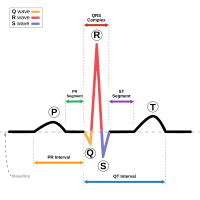
We read the article entitled ‘‘Short-term outcome of acute inferior wall myocardial infarction (IWMI) with emphasis on conduction blocks: a prospective observational study in Indian population’’ by Kumar et al. (1) published in Anatol J Cardiol 2017; 17: 229-34 with great interest. In this study, the authors have reported that the mortality rate was higher in patients with conduction blocks than in subjects without conduction blocks. According to the study, subjects with IWMI were not enrolled homogenously since some subjects did not receive reperfusion therapy, including thrombolytic therapy and in some subjects, coronary angiography was not performed at follow-up. The rate of thrombolytic therapy in the group with conduction block was statistically lower than in the group without conduction block. Further analyses may be performed to understand the relation of conduction defects with mortality due to the fact that thrombolytic therapy has the ability to reduce mortality. In this context, data from prefibrinolytic and fibrinolytic eras are also needed for further analyses of subjects with conduction defects. However, changes and developments in the medications of IWMI in the last 30 years may lead to confusion in comparison of the related study results. Even so, the presence of conduction defects in the group receiving thrombolytic therapy seemed to be higher than expected compared with previous literature (2). One of the reasons contributing to this result may be the lack of data regarding the use of AV node-blocking drugs, such as beta-blockers, nondihydropyridine calcium blockers, and antiarrhythmic drugs, before IWMI. Additionally, although electrocardiography (ECG) is a simple and rapid method to detect the presence of right ventricle myocardial infarction (RVMI) with IWMI, ECG findings can be unremarkable in the following hours of successful or unsuccessful reperfusion. In one study, electrocardiography detected less than half of the patients with RVMI who were shown to have right ventricle (RV) involvement by magnetic resonance imaging (3). However, echocardiography is a reproducible, commonly used diagnostic modality, and the presence of RVMI was shown more reliably by using different echocardiographic parameters such as RV dilatation, RV wall hypokinesia/akinesia, RV wall motion index, RV fractional area change, tricuspid annular plane systolic excursion, tissue Doppler imaging (S and E waves), and myocardial strain/strain rate. Some of these parameters may also play an important role in determining prognosis and treatment strategies (4). In this study, there was no report of results related to echocardiographic evaluation of RV. Relying solely on ECG may not correctly reflect the severity of RV involvement. Thus, clinical outcomes may not be predicted appropriately. Right atrial (RA) ischemia is not uncommon in RVMI. In the presence of RVMI, mechanical activity increase of the atrium tries to compensate cardiac output and improve prognosis in systolic and diastolic functions of RV under ischemia. When RA ischemia develops, it may further compromise RV ischemia due to the loss of compensating mechanism, and the development of rate and rhythm disturbances, particularly in patients with proximal right coronary artery occlusion (5). It would be better for the readers to mention the role of RA ischemia in patients with RVMI in the discussion section to contribute the understanding of in-hospital worse outcomes.
Journal Title: Anatolian Journal of Cardiology
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!