Photo from wikipedia
EJD, vol. 30, n◦ 4, July-August 2020 December 2019 and 8th January 2020, respectively. A relapse of skin manifestations involving the face, neck, trunk and inferior extremities was apparent in… Click to show full abstract
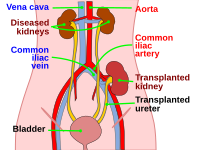
EJD, vol. 30, n◦ 4, July-August 2020 December 2019 and 8th January 2020, respectively. A relapse of skin manifestations involving the face, neck, trunk and inferior extremities was apparent in February 2020, when the woman was hospitalized, complaining of intense pain at the site of the transplanted kidney, and was admitted to surgery for explant of the organ. Progressive worsening of bullous lesions led to widespread skin involvement two weeks after the explant (figure 1A). The diagnosis of BP was confirmed by histopathology showing dermo-epidermal cleavage and direct immunofluorescence findings demonstrating deposits of C3, IgG and C1q along the basement membrane zone and hair bulb wall (figure 1B). MESACUP ELISA assay (MBL Co, Nagoya, Japan) for serum anti BP180 autoantibodies detected a positive value of 65.07 U/mL (normal value < 9 U/mL). Oral prednisone, as 0.5 mg/kg daily therapy, was started during the stay at the hospital and continued after the patient had been discharged. Skin examination showed almost complete resolution of skin disease after one month of treatment. Previous reports indicate that BP and graft rejection might be related events rather than casually associated diseases with no mutual correlation. Four possible temporal and/or causal associations have been proposed: a) BP during allograft rejection, b) BP subsequent to withdrawal of immunosuppression, c) BP triggered by drugs or infections, and d) BP in the setting of dialytic therapy [5]. BP occurring during rejection may be explained by a possible link between basement membrane zone and kidney antigens responsible for an epitope-spreading phenomenon [6, 7]. Immunosuppressant regimens in transplant recipients could also mask pre-existent BP [8]. Furthermore, withdrawal from immunosuppression may determine a boost in immune function and trigger autoimmunity responsible for the onset or the rebound of BP [8]. As far as drug-induced BP is concerned, only mTOR inhibitors have been reported to induce BP in renal transplant recipients [9]. The explant of the rejected organ in our patient was not associated, as expected, with remission of the autoimmune bullous disease, but we observed an increase in severity and extent of disease indicating that the rejection may have induced a sustained immune response against common antigens [7, 9]. In our patient, blistering skin lesions, presenting concomitant with graft rejection, were not acknowledged as signs of BP at first, due to remission after an immunosuppressive graft-saving attempt. However, it is likely that subsequent abrupt suspension of immunosuppressive treatment following rejection precipitated the previously unrecognized autoimmune disorder, together with persistent immune system activation against the rejected kidney. Therefore, care should be taken in tapering immunosuppressive treatment even after rejected organ is explanted since a sustained immune response may lead to escalation in the severity of potentially related autoimmune processes.
Journal Title: European Journal of Dermatology
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!