Photo from wikipedia
Subarachnoid haemorrhage is a known but rare manifestation of cerebral venous and dural sinus thrombosis. We present a case of a 62-year-old female with stable Crohn’s disease, who developed thunderclap… Click to show full abstract
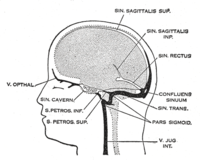
Subarachnoid haemorrhage is a known but rare manifestation of cerebral venous and dural sinus thrombosis. We present a case of a 62-year-old female with stable Crohn’s disease, who developed thunderclap headache with nausea. Upon presentation, she had no meningism and her neurological examination was normal. Unenhanced computed tomography (CT) revealed a small subarachnoid haemorrhage in the right ambient cistern, extending above the right cerebral convexity. CT angiography did not demonstrate an arterial aneurysm. The patient was admitted to the neurology ward with a working diagnosis of nonaneurysmal subarachnoid hemorrhage. A few days later she developed mild right abducens palsy and blurred vision. Fundoscopy revealed bilateral papilledema. A repeated CT scan with CT venography revealed a thrombosis of the transverse and sigmoid sinuses as well as the jugular vein, pronounced particularly on the right side. Thrombophilia testing was positive for activated protein C resistance in the heterozygous form. We instituted anticoagulation with therapeutic doses of low molecular weight heparin. The clinical course of the thrombosis was favourable. Crohn’s disease, especially in combination with inborn thrombophilia, could represent a prothrombotic state. This may be associated with the thrombosis in our patient. In cases of an unusually localised subarachnoid haemorrhage in the absence of an arterial aneurysm, CT venography should be performed to rule out cerebral venous and dural sinus thrombosis.
Journal Title: Journal of Neuropathology and Experimental Neurology
Year Published: 2017
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!