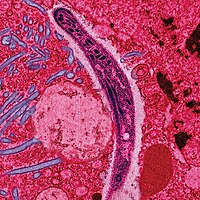
Photo from wikipedia
Purpose To investigated the effectiveness of antiplatelet agents for the secondary prevention of stroke according to CYP2C19 genotype in patients with ischemic stroke (IS). Methods Between August 2009 and December… Click to show full abstract
Purpose To investigated the effectiveness of antiplatelet agents for the secondary prevention of stroke according to CYP2C19 genotype in patients with ischemic stroke (IS). Methods Between August 2009 and December 2011, 570 acute IS patients with acute large-artery atherosclerosis were randomly assigned to receive either combined clopidogrel and aspirin for the first 30 day, and clopidogrel thereafter (clopidogrel group, n=284) or aspirin monotherapy (aspirin group, n=286). CYP2C19 genotypes were measured and masked until the end-of-study. The primary outcome was a composite of IS, transient ischemic attack (TIA), myocardial infarction (MI), and death. Results During the 5 years follow-up, the primary outcome occurred in 105 patients (18.4%) (71 had IS, 10 had TIA, 12 had MI, and 12 died). There were no significant differences in the primary outcome between clopidogrel group and aspirin group (16.5% vs. 20.3%) or between carriers of the CYP2C19 reduced-function alleles and noncarriers (21.8% vs.15.7%). In patients with aspirin therapy, CYP2C19 polymorphism was not associated with the primary outcome. However, in patients treated with clopidogrel, carriers of at least one CYP2C19 reduced-function allele had a 3-fold higher adjusted risk for primary outcome compared with noncarriers (95% confidence interval, 1.23 to 8.74). Conclusions Among IS patients treated with clopidogrel, carriers of a reduced-function CYP2C19 allele had a significantly higher rate of adverse vascular events than did noncarriers. It should avoid prescribing clopidogrel to these patients with known CYP2C19 polymorphisms.
Journal Title: Oncotarget
Year Published: 2018
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!