Photo from wikipedia
Lateral lumbar interbody fusion (LLIF) is used to treat various pathological conditions because it reduces surgical invasiveness and bleeding and has an indirect decompressive effect, with strong corrective force. However,… Click to show full abstract
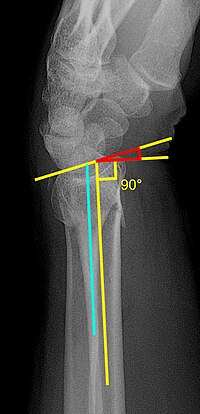
Lateral lumbar interbody fusion (LLIF) is used to treat various pathological conditions because it reduces surgical invasiveness and bleeding and has an indirect decompressive effect, with strong corrective force. However, a drawback is the complication rate, which is reported to be as high as 26.7%. Reported complications include abdominal problems, neurological symptoms, psoas weakness, vascular injury, and anterior longitudinal ligament (ALL) injury. ALL injury is usually not detected intraoperatively but becomes evident after surgery. We encountered a case of anterior opening due to an ALL avulsion fracture when changing the patient’s position from lateral to prone during extreme lateral interbody fusion (XLIF) surgery. A 72-year-old woman presented to our hospital after several years of low back pain, pain in the right buttock and lateral thigh, and intermittent claudication, with no muscle weakness. Magnetic resonance imaging showed canal stenosis at L3/4 (Fig. 1), while X-ray imaging showed L3/4 lateral disk mobility of 3° and lumbar kyphosis. Computed tomography (CT) revealed osseous bridging of the vertebrae from L2 to L3 and from L4 to the sacrum. We planned XLIF at L3/4 and lumbar fixation from L2 to L5 using percutaneous pedicle screws (PPSs). XLIF at L3/4 was performed in the right lateral position. A cage, with a height of 9 mm, was inserted, with no complications. Next, we changed the patient’s position from lateral to prone. Fluoroscopy then revealed an anterior opening at L3/4 (Fig. 2). To apply compression more easily to the opening, we switched to open surgery for pedicle screw insertion. After inserting the screws, we applied compression at this level. Postoperative CT images revealed an ALL avulsion fracture (Fig. 3). As of 1 year later, the postoperative course has been excellent. The frequency of ALL injury during anterior-posterior correction of spinal deformity by LLIF is as high as 21.1%41.2%. ALL injuries are more likely to occur in cases where the disk height is 5 mm, the cage is placed anteriorly, or the deformity is strongly corrected. ALL injury may result in reduced anterior support and increase the risk of nonunion and rod breakage. Although most cases occur during corrective posterior surgery, ALL injury can also occur when a cage is inserted during anterior surgery. ALL rupture should be suspected if interbody tension disappears during the interbody procedure. In this case, we were able to feel the tension of the ALL during anterior surgery. To our knowledge, there have been no reports of ALL avulsion fracture due to a positional change in the patient. The problem with the fusion of several vertebrae is that the mobility of the spine is reduced, and mechanical stress tends to concentrate in areas where the continuity of ligament ossification is interrupted. In our case, due to the osseous bridging of the vertebrae from L2 to L3 and from L4 to the sacrum, it is likely that mechanical stress at L3/4 after the positional change. Considering the cause of the stenosis at L3/4 and the presence of lumbar kyphosis and osteoporosis, we antici-
Journal Title: Spine Surgery and Related Research
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!