Photo from wikipedia
Classical or BCR-ABL1 negative myeloproliferative neoplasms (MPN) are clonal diseases originating from the acquisition at the stem cell level of a phenotype driver mutation affecting JAK2, MPL or CALR genes.… Click to show full abstract
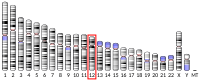
Classical or BCR-ABL1 negative myeloproliferative neoplasms (MPN) are clonal diseases originating from the acquisition at the stem cell level of a phenotype driver mutation affecting JAK2, MPL or CALR genes. MPN are comprised of three illnesses: essential thrombocythemia (ET), polycythemia vera (PV) and primary myelofibrosis (PMF). These diseases are characterized by recurrent complications including severe thromboembolic events and secondary transformation to myelofibrosis or acute myeloid leukemia (AML). Large efforts have been undertaken to better define the prognosis of MPN patients and understand the reasons for the heterogeneous clinical evolution among these patients. Thanks to the development of next-generation sequencing (NGS) techniques, additional molecular alterations have been discovered and considered in the delineation of risk categories in MPN. For example, some high risk mutations have been identified and most studies highlighted that the presence of a high number of mutations in a single patient is correlated to poorer outcome. The most frequent mutations are found in genes regulating epigenetics, intracellular cell signaling, transcription factors or the spliceosome, making the regulation of gene expression the main target of the molecular alterations identified in MPN. The CCND2 gene on chromosome 12 encodes the cyclin D2 cell cycle regulator which has been shown to be deregulated in cancer. Cyclin D2 overexpression has been reported in solid tumors. In hematopoietic malignancies, translocations involving the CCND2 gene are found in lymphomas while mutations in the CCND2 gene have been reported in AML, mainly in core-binding factor AML. Finally, de novo germline CCND2 mutations are causative for a malformation syndrome called megalencephaly-polymicrogyria-polydactyly-hydrocephalus (MPPH). Interestingly, both the mutations reported in cancer and in MPPH target a very narrow region coding for amino acids between Gln265 and Val284 with a hotspot on Thr280 and Pro281 which are conserved amino acids involved in cyclin D2 degradation. The reported mutations are either missense or nonsense mutations which have been shown to increase the stability of cyclin D2 and hence the cellular proliferation. As CCND2 mutations have recently been described in one patient with triple-negative PMF and four patients with atypical chronic myeloid leukemia (aCML) or myeloproliferative neoplasms unclassifiable (MPNu), we aimed at evaluating the frequency of such mutations in a large cohort of MPN patients. We prospectively screened 708 samples from 589 patients with classical MPN (233 ET; 187 PV; 169 MF) using a capture-based custom NGS panel (Sophia Genetics) targeting 36 myeloid genes (ABL1; ASXL; BRAF; CALR; CBL; CCND2; CEBPA; CSF3R; CUX1; DNMT3A; ETNK1 ; ETV6; EZH2; FLT3; HRAS; IDH1; IDH2; IKZF1; JAK2; KIT; KRAS; MPL; NFE2; NPM1; NRAS; PTPN11; RUNX1; SETBP1; SF3B1; SH2B3; SRSF2; TET2; TP53; U2AF1; WT1; ZRSR2). Of note, the full coding sequence of the CCND2 gene was captured. Libraries were prepared on libraries were prepared on 200 ng DNA extracted from whole blood (Qiagen) and the sequencing was performed on a MiSeq instrument (Illumina). Bioinformatics were composed at Sophia Genetics (Switzerland) using the SOPHIA DDM software and significant variants were retained with a sensitivity of 1%. The study was accepted by the local Institutional Review Board and patients gave informed consent for the study. The driver mutations were present with frequencies similar to those reported in the literature (Table 1). Whereas PV patients were found positive for JAK2mutations (90% of JAK2 V617F and 2% of exon 12 mutations), ET and MF patients were positive for JAK2 V617F (53% in both groups), MPL exon 10 (4% and 8% respectively) or CALR exon 9 mutations (26% and 27% respectively). Apart from the driver mutation, the most frequently found additional mutations targeted the TET2, DNMT3A and ASXL1 genes (Table 1). We found CCND2 mutations at low variant allelic frequencies (VAF) in four patients (0.7% of our cohort), one with PV, one with MF and two with ET (Table 2). The mutations identified were missense mutations at hot-spot amino acids Thr280 and Pro281 and one nonsense mutation (p.Ser271*). The driver mutations present in these four patients included CALR, JAK2 and MPL mutants, excluding a possible association with one particular driver gene. Of note, the CCND2 mutation was present as the only additional mutation in two patients whereas two to four additional mutations were present in one ET and one MF patient respectively (Table 2). We had the opportunity to analyze three sequential samples over 15 months in one patient with MF (#4). We observed that the CCND2 mutant VAF significantly increased from 2.4% to 5.1%, while the patient WAS under treatment with ruxolitinib. This patient did not present evidence of disease progression during these 15 months. It is nowadays largely acknowledged that variability in patients’ prognosis is mainly explained by the pattern of acquired molecular alterations that may be very different from one patient to another. A clonal evolution of the
Journal Title: Haematologica
Year Published: 2020
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!