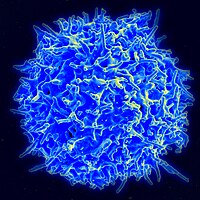
Photo from wikipedia
In Argentina, the human T-cell lymphotropic virus type 1 (HTLV-1) infection has been documented mainly among blood banks with a prevalence of ~0.02–0.046% for Buenos Aires city, 0.8% for the… Click to show full abstract
In Argentina, the human T-cell lymphotropic virus type 1 (HTLV-1) infection has been documented mainly among blood banks with a prevalence of ~0.02–0.046% for Buenos Aires city, 0.8% for the northeast, and 1% for the northwest; both areas are considered endemic for HTLV-2 and 1, respectively. Policies and specific guidelines for testing blood donors for HTLV are included since 2005. Screening for antibodies is performed at blood banks and confirmatory testing is performed at reference laboratories. There are no specific recommendations for the assistance of communities and individuals affected, nor referral to specialized clinics on the HTLV infection. In 2016, as a strategy of intervention, we opened a specialized clinical attendance in a referral infectious diseases public hospital for the comprehensive approach to patients with HTLV, offering follow-up and counseling for patients and their families for the early diagnosis of HTLV-1/2 and related diseases. During the study, 124 patients with presumptive HTLV positive diagnosis from blood bank, symptomatic patients (SPs), relatives, and descendants visited the unit. A total of 46 patients were HTLV positive (38 HTLV-1 and 8 HTLV-2). There were nine SPs (2 adult T-cell leukemia/lymphoma [ATL] and 7 HTLV-1-associated myelopathy/tropical spastic paraparesis [HAM/TSP]). All patients with HTLV-1 and−2 were offered to study their relatives. Two out of 37 (5.4%) descendants tested were positive for HTLV-1. Sexual partners were studied; among 6 out of 11 couples (54.5%) were found positive (5 HTLV-1 and 1 HTLV-2). Other relatives, such as mothers (1/2) and siblings (1/6), were positive for HTLV-1. According to the place of birth among HTLV-1 carriers, 58% were born in an endemic area or in countries where HTLV infection is considered endemic while for HTLV-2 carriers, 12.5% were born in an endemic area of Argentina. The proviral load (pVL) was measured in all, patients with HTLV-1 being higher in symptomatic compared with asymptomatic carriers. In addition, two pregnant women were early diagnosed during their puerperium and breastmilk replacement by formula was indicated. Inhibition of lactation was also indicated. Our study provides tools for a multidisciplinary approach to the infection and reinforces the importance of having specialized clinical units in neglected diseases, such as HTLV for counseling, clinical and laboratory follow-up, and providing useful information for patients for self-care and that of their families.
Journal Title: Frontiers in Medicine
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!