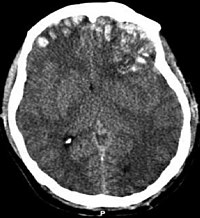
Photo from wikipedia
Objective To determine whether, in patients undergoing rehabilitation after traumatic or hemorrhagic brain injury, seizures and the use of antiepileptic drugs (AEDs) negatively impact on functional outcome, and, in turn,… Click to show full abstract
Objective To determine whether, in patients undergoing rehabilitation after traumatic or hemorrhagic brain injury, seizures and the use of antiepileptic drugs (AEDs) negatively impact on functional outcome, and, in turn, whether prophylactic AED therapy can prevent the development of seizures. Design Observational retrospective study. Setting Highly specialized inpatient neurorehabilitation clinic. Participants Patients with traumatic brain injury (TBI), or hemorrhagic stroke (HS) consecutively admitted to our neurorehabilitation unit between January 1, 2009, and December 31, 2018. Main measures and variables Patients' demographic data, neurological status (Glasgow Coma Scale), and rehabilitation outcome (Functional Independence Measure scale), both assessed on admission and on discharge, associated neurosurgical procedures (craniectomy, or cranioplasty), AED use, early or late seizures occurrence, and death during hospitalization. Results Of 740 patients, 162 (21.9%) had seizures, and prophylactic AEDs were started in 192 (25.9%). Multivariate logistic regression identified severity of brain injury as a risk factor for acute symptomatic seizures (ASS) in HS (OR = 1.800, 95%CI = 1.133–1.859, p = 0.013), and for unprovoked seizures (US) in TBI (OR = 1.679, 95%CI = 1.062–2.655, p = 0.027). Prophylaxis with AEDs reduced ASS frequency, but, if protracted for months, was associated with US occurrence (HS, p < 0.0001; TBI, p = 0.0002; vs. untreated patients). Presence of US (β = −0.12; p < 0.0001) and prophylaxis with AEDs (β = −0.09; p = 0.002), were associated with poor functional outcome, regardless of age, severity of brain insult, and HS vs. TBI subtype. Conclusions Severity of brain injury and occurrence of seizures during neurorehabilitation are the main driver of poor outcome in both HS and TBI. The possible detrimental role on the epileptogenic and functional outcome played by seizures prophylaxis with AEDs, nonetheless useful to prevent ASS if administered over the first week after the brain injury, warrants further investigation.
Journal Title: Frontiers in Neurology
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!