Photo from wikipedia
A PubMed search using the terms “vitamin D and COVID-19” reveals more than 1,000 papers. Mostly they indicate a correlation between a low level of vitamin D and a severe… Click to show full abstract
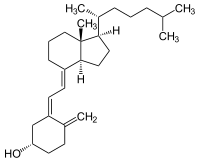
A PubMed search using the terms “vitamin D and COVID-19” reveals more than 1,000 papers. Mostly they indicate a correlation between a low level of vitamin D and a severe outcome from COVID-19 disease (Grant et al., 2022). However, it is easy and quite common in medicine to confound causality with a simple correlation. Moreover, such confusion is particularly plausible for vitamin D research. The problem arises from naming vitamin D a “vitamin,” whereas, in fact, it is a hormone that is produced when the human skin is exposed to sunlight. Therefore, vitamin D is more likely to be produced in people who are fit enough to spend time outdoors. Consequently, a proper blood level of vitamin D is much more likely in fit and healthy people than in sick people. The best means of differentiating a random correlation from causal inference is to describe the underlying mechanism (Pearl and Mackenzie, 2019). The active metabolite of vitamin D is the steroid hormone 1,25-dihydroxyvitamin D (1,25D) (Carlberg, 2014a). Vitamin D is produced from 7-dehydrocholesterol when the human skin is exposed to UV light. Then, vitamin D activation occurs in two steps: 25-hydroxylation followed by 1α-hydroxylation (Prosser and Jones, 2004). The first step occurs in the liver, where vitamin D undergoes hydroxylation to 25-hydroxyvitamin D (25D). 25D undergoes hydroxylation in the kidneys to the highly active metabolite 1,25D. Both 25D and 1,25D circulate in the blood via the vitamin D binding protein (DBP). 25D bound to DBP has a long half-life of around 2–3 weeks, whereas 1,25D has a short half-life of 10–20 h (Carter, 2011). Hence, serum 25D concentration is used routinely to measure the vitamin D status in the human body (Sempos et al., 2012). Hydroxylation of 1,25D at carbon atom C-24, catalyzed by 24-hydroxylase of 1,25D (CYP24A1), is the first step of its inactivation. A view is that the CYP24A1 level is downregulated by sex hormones and that a higher level of 17β-estradiol may enhance the actions of 1,25D. Peruzzu et al. presented data to support this mechanism. Vitamin D deficiency is perhaps the most common nutritional deficiency in the world. Recently, there has been increasing awareness of vitamin D deficiency, and its supplementation is now much more common, but seldom regularly controlled. Regarding vitamin D deficiency, the currently agreed levels of serum 25D are deficiency at< 12 ng/ml, insufficiency at 12–20 ng/ml, and levels between 20 and 50 ng/ml are considered to be adequate. In their article, Hafez et al. reported that vitamin D deficiency does correlate significantly with higher mortality from COVID-19. The receptor for 1,25D is the vitamin D receptor (VDR), which, upon binding to the ligand, translocates from the cytoplasm to the cell nucleus. There, VDR acts as a ligand-activated transcription factor to regulate the transcription of its target genes (Aranda and Pascual, 2001). Hundreds of genes are regulated by VDR (Pike and Meyer, 2014); many of them are responsible for Edited and reviewed by: Salvatore Salomone, University of Catania, Italy
Journal Title: Frontiers in Pharmacology
Year Published: 2022
Link to full text (if available)
Share on Social Media: Sign Up to like & get
recommendations!